Robert Whitcomb: How to Speed Up Infrastructure Repair
An irritated citizenry has blocked a bid by the Pawtucket Red Sox, employing very few people and with a mostly seasonal business, to grab valuable public land and erect, with lots of public money, a stadium in downtown Providence, on Route 195- relocation land. The plan would have involved massive tax breaks for the rich PawSox folks that would have been offset by mostly poorer people’s taxes.
The public is belatedly becoming more skeptical about subsidizing individual businesses. (Now if only they were more skeptical about casinos’ “economic- development’’ claims. Look at the research.)
Perhaps Lifespan will sell its Victory Plating tract to the PawSox. And maybe a for-profit (Tenet?) or “nonprofit’’ (Partners?) hospital chain will buy Lifespan, which faces many challenges. Capitalism churns on!
In any event, the stadium experience is a reminder that we must improve our physical infrastructure, in downtown Providence and around America.
Improved infrastructure will be key to a very promising proposal by a team comprising Baltimore’s Wexford Science & Technology and Boston’s CV Properties LLC for a life-sciences park on some Route 195-relocation acres. This could mean a total of hundreds of well-paying, year-round jobs in Providence at many companies. Tax incentives for this idea have merit. (I’d also rather fill the land slated for a park in the 195 area with other job-and-tax-producing businesses, but that’s politically incorrect.)
The proximity of the Alpert Medical School at Brown University, the Brown School of Public Health, hospitals and a nursing school is a big lure. Also attractive is that Providence costs are lower than in such bio-tech centers as Boston-Cambridge and that the site is on the East Coast’s main street (Route 95, Amtrak and an easy-to-access airport).
Rhode Island’s decrepit bridges and roads are not a lure. Governor Raimondo’s proposal for tolls on trucks (which do 90 percent of the damage to our roads and bridges) to help pay for their repair, and in some cases replacement, should have been enacted last spring. It’s an emergency.
It takes far too long to fix infrastructure, be it transportation, electricity, water supply or other key things. The main impediment is red tape, of which the U.S. has more than other developed nations. That’s why their infrastructure is in much better shape than ours.
Common Good sent me a report detailing the vast cost of the delays in fixing our infrastructure and giving proposals on what to do. It has received bi-partisan applause. But will officials act?
The study focuses on federal regulation, but has much resonance for state policies, too. And, of course, many big projects, including the Route 195-relocation one, heavily involve state and federal laws and regulations.
Among the report’s suggestions:
* Solicit public comment on projects before (my emphasis) formal plans are announced as well as through the review process to cut down on the need to revise so much at the end, but keep windy public meetings to a minimum.
* Designate one (my emphasis) environmental official to determine the scope and adequacy of an environmental review in order to slice away at the extreme layering of the review process. Keep the reports at fewer than 300 pages. The review “should focus on material issues of impact and possible alternatives, not endless details.’’ Most importantly, “Net overall (my emphasis) impact should be the most important finding.’’
* Require all claims challenging a project to be brought within 90 days of issuing federal permits.
* Replace multiple permitting with a “one-stop shop.’’ We desperately need to consolidate the approval process.
Amidst the migrants flooding Europe will be a few ISIS types. That there are far too many migrants for border officials to do thorough background checks on is scary.
Fall’s earlier nightfalls remind us of speeding time. When you’re young, three decades seem close to infinity, now it seems yesterday and tomorrow. I grew up in a house built in 1930, but it seemed ancient. (My four siblings and I did a lot of damage!) Yet in 1960, when I was 13, the full onset of the Depression was only 30 years before. The telescoping of time.
Robert Whitcomb: Private-sector passenger rail?
Since the disappearance of private-sector passenger rail service decades ago, intrepid entrepreneurs have tried to bring it back. None have succeeded.
However, in some densely populated places, passenger rail has even thrived in the public sector, at least as measured by passenger volume. This mostly means Amtrak in the Northeast Corridor and several major cities’ long-established commuter-rail networks. But new commuter rail is also catching on in some unlikely places, including such Sunbelt cities as Dallas and Phoenix, which now have popular light-rail systems.
Now, with an aging population, the proliferation of digital devices that many people would prefer to stare at rather than at the road and the increasing unpleasantness of traveling on America’s decaying highway infrastructure amidst texting and angry drivers, private passenger rail looks more capitalistically attractive.
Consider All Aboard Florida, a company that plans to offer extensive rail service starting in 2017. It will connect Miami and Orlando in just under three hours, with stops in Fort Lauderdale and West Palm Beach.
Its advertising copy eloquently describes commuter rail’s allure in populous areas: “{Y}ou can turn your stressful daily {car} commute into a productive or peaceful time by choosing to take the train instead of driving your car. By becoming a train commuter, you’ll also help the economy and environment while you’re at it.’’
Southern New England, like much of Florida, is densely populated, with some unused or underused rail rights of way. So our entrepreneurs occasionally propose private passenger rail for routes not served by Amtrak or such regional mass-transit organizations as Metro North and the Massachusetts Bay Transportation Authority.
Consider the Worcester-Providence route, on which a new company called the Boston Surface Railroad Co. wants to start operating commuter rail service in 2017 on the (now freight-only) Providence and Worcester Railroad’s tracks. Most of the commuters going to work would be traveling from the Worcester area, via Woonsocket, where there would be a stop, to Greater Providence. While Providence itself has fewer people -- about 178,000 -- than Worcester (about 183,000), the two-state Providence metro area -- about 1.6 million -- is much bigger than the latter’s metro area’s about 813,000.
The density is there for rail service. That the region has an older population than the national average and frequent bad winter weather also give the idea a lift.
But the old rail line needs to be upgraded if the trips are to be made fast enough to lure many travelers. The company hopes to offer a one-way time of about 70 minutes on a route that you can drive in about 45 minutes in moderate traffic and clement weather. That could be a killer.
What this project and similar ones need is new welded track, rebuilt rail beds (with help of public money?) and some entirely new routes to make service competitive with car-driving times. We need more passenger and duel-purpose passenger-freight rail lines, not more highways. But getting them will be tough in a country that so blithely tolerates crumbling transportation infrastructure and has a deeply entrenched libertarian commuting habit of a single person driving long distances to work. Unless gasoline tops $5 a gallon and stays there for at least a year, it’s hard to see millions of Americans deciding that they’ll quit their cars to take the train.
Still, I applaud the project’s CEO, Vincent Bono, and hope that thousands of commuters will give his railroad a try. While the trip would be long, think of how much uninterrupted Web surfing (free Wi-Fi!), reading and snoozing you could get on these trains, with their reclining seats.
xxx
An Aug. 10 USA Today story was headlined “Smaller cities emerge among top picks for biz meetings.’’ Depressingly, Providence was not on the list of the top 50 places for “meetings and events’’ in 2015, say evaluations by Cvent. But many far less interesting and attractive places were.
The reasons probably include Rhode Island’s under-funded and balkanized self-promotion and the long delay (now finally being addressed) in building a longer runway at T.F. Green Airport.
Robert Whitcomb (rwhitcomb51@gmail.com), a Providence-based editor, writer and consultant, oversees newenglanddiary.com and is a partner in Cambridge Management Group, (cmg625.com), a healthcare consultancy, and a fellow at the Pell Center. He used to be the editorial-page editor of The Providence Journal and the finance editor of the International Herald Tribune, among other jobs.
Robert Whitcomb: Drawbacks of deregulation and DIY
For years, deregulation and the Internet have been pulling us into a more decentralized and freelance economy, in which there’s wider consumer choice, albeit with stagnant pay and a decline in person-to-person service that forces us to do more tasks ourselves that were previously done by those dinosaurs called “employees’’.
Consider Uber. As I discovered when one of my daughters pulled out her iPhone a couple of years ago on a busy Manhattan street to summon an Uber driver, it’s sometimes faster to find one of these mobile freelancers than it is to find a regulated Yellow Cab in a big city.
But the cabs, being regulated, function as a public utility. They have to meet certain basic minimums of availability, cleanliness and safety that can’t be imposed on the likes of Uber, whose drivers are, of course, not obligated to provide services in the same way as cabbies. I don’t think that we want unregulated drivers to totally replace generally reliable and regulated cabbies.
Long before Uber, of course, there was the partial deregulation of the airlines. While this led initially to lower prices for many travelers, it has also made travel more chaotic and unpredictable. And deregulation, the “Hub-and-Spoke’’ system and relentless airline mergers mean that mid-size cities get shorted on flights.
While better electronics systems make planes less likely to crash these days than three decades ago, air travel itself is increasingly miserable.
In the old, tightly regulated days, figuring out airline schedules and fares was comparatively easy. Now it’s an ordeal, and conditions within airplanes are increasingly crowded and unhealthy. And as the airlines, like other businesses, seek to outsource service to computers so that they can lay off more people, addressing problems by communicating with customer-service humans gets tougher.
Then there’s the new do-it-yourself, deregulated and decentralized energy world. Consider that many affluent folks are saving money and reducing their carbon footprints by having solar panels installed on their roofs. Good in itself! But this takes business away from the utility companies, which could jeopardize the viability of the huge electric grids that utilities maintain. We’ll continue to need that grid to support modern society, with its ever-increasing supply of electronic devices.
Might not it be better if we put more focus on producing green electricity with huge solar-panel arrays and wind-turbine farms maintained by utilities that serve everyone – rich and poor?
xxx
The Obama administration has worked very hard to craft a deal with Iran to try to get it to at least postpone continued work on nuclear weapons.
But the administration’s effort will probably turn out to have been in vain. For one thing, the corrupt theocratic dictatorship that runs Iran will cheat and cheat as it evades inspections. It may receive technical help in this cheating from the likes of fellow police states Russia and China, two of the signatories to the nuclear deal, which will happily sell them militarily useful stuff.
Iran will almost certainly use the billions of dollars freed up by the ending of economic sanctions to increase its troublemaking. Iran’s regime seeks to dominate the Mideast – partly to protect and promote its fellow Shiites and partly because domination is fun and profitable for its leaders. And Tehran hasn’t really toned down its “Death to America and Israel’’ rhetoric.
Now we have made the mullahs more macho. No wonder Iran’s neighborhood is scared.
Some complain that America, as the first nuclear power, is hypocritical in trying to keep nuclear weapons out of the hands of other nations. That seeks to make an equivalence between a democratic nation like America and a dictatorship like Iran. And remember why we started our nuclear-weapons program in the first place – to defend ourselves from Germany’s mass-murdering Nazi regime, which was working hard to create an atomic bomb.
Some say that expanding trade with Iran will somehow make it kindlier. They said that about Germany before World War I and China now. Nations have other reasons besides economics to be nasty – for instance, paranoia, power for the sake of power and religion.
Robert Whitcomb (rwhitcomb51@gmail.com) oversees New England Diary. He's also a Fellow at the Pell Center, in Newport, and a partner at Cambridge Management Group (cmg625.com), a healthcare-sector consultancy. He used to be the editorial-page editor of The Providence Journal, the finance editor of the International Herald Tribune and an editor at The Wall Street Journal, among other jobs.
Robert Whitcomb: Health-care beacons, Snowden, our big river
The Connecticut River at Orford, N.H. (See item at bottom.)
Much of American health care’s future can be seen in two synergistic kinds of institutions in Rhode Island.
One is Federally Qualified Health Centers (FQHCs). These facilities, set up around America, provide a wide range of free and insurance-subsidized clinical help for millions of patients, most of them low-income. The other is Johnson & Wales University’s spanking new Center for Physician Assistant Studies.
Consider the state’s biggest FQHC organization -- Providence Community Health Centers (PCHC). Its teams of physicians and other clinicians, such as nurses and nurse practitioners, work for what is the biggest single provider of primary-care services in Providence, with more than 35,000 patients. (I toured PCHC’s immaculate Prairie Avenue campus the other week, led by Merrill Thomas, its CEO, and Jane Hayward, the Rhode Island Health Center Association’s president.)
PCHC ‘s mission, it says, is to “provide neighborhood-based high quality and accessible primary medical care to improve the health status of the residents of Providence and surrounding communities regardless of their ability to pay.’’ FQHCs play especially important roles in inner cities and impoverished rural areas, such as Appalachia, where many physicians don’t want to practice, especially because of low reimbursement and so many difficult cases involving seemingly intractable behavioral-health issues.
Expanding primary care -- especially preventive care -- is essential if America is to improve overall health outcomes that are near the bottom of the Developed World while better controlling medical costs, which are the highest.
Whatever happens with the Affordable Care Act, the U.S. population’s aging (older means sicker); the daunting complexity of our health-insurance system; the permanent exit of many well-paying jobs; emigration to the United States of low-income people, and the decline of the stable, two-resident-parent family suggest that Federally Qualified Health Centers ought to play even bigger roles.
Of course, increasing the numbers of primary-care clinicians is essential for the long-term success of these clinics. Doing just that is the Johnson & Wales Center for Physician Assistant Studies, which has a beautiful building in Providence’s Jewelry District. George Bottomley, its director, gave me a tour the other week.
Its 24-month master’s program addresses the need to train many more non-physician clinicians who can perform highly professionally and cost-effectively some of the tasks now performed by over-worked (if highly paid) doctors. PAs are especially useful in getting patients to make the behavioral changes needed to prevent serious illness, in part because they can generally spend more time with patients than can physicians; many of the latter are more harried than ever because of onerous electronic-health-record duties and administrative pressures to boost patient volume.
J&W notes that PAs work in integrated medical teams to “provide diagnostic, therapeutic and preventive health-care services.’’ (By the way, the differences between physician assistants and nurse practitioners mostly involve some education details. They’re very similar professions.)
With physicians as supervisors, physician assistants take patients’ histories and perform exams; order lab tests; prescribe medications; diagnose illnesses; develop treatment plans, and counsel and educate patients.
No wonder that demand for PAs is surging. Forbes.com has listed Physician Assistant Studies as the “No. 1 Best Master’s Degree for Jobs.’’ The American Academy of Physician Assistants (AAPA.org) says that “demand for physician assistants and nurse practitioners rose by more than 300 percent in the last three years.’’
We’ll need Johnson & Wales PAs in droves in coming years as, technology, demographics and new cost controls continue to transform U.S. health care for all patients, especially in primary care, in which physician assistants will be at the forefront.
xxx
Edward Snowden – as a Russian spy and/or as an arrogant but naïve narcissist-- has provided vast amounts of U.S. security information to Vladimir Putin’s police state, perhaps resulting in the death of agents working for us. And he has aided the Chinese dictatorship’s relentless cyber-warfare against America. Some hero!
xxx
Last week we cruised the gorgeous Upper Connecticut River on a pontoon boat. Because it’s by far New England’s biggest river, on it you get a sense of what Mark Twain might have felt on the Mississippi. We yakked desultorily in the soft breeze about big projects we’d do – as if we were 30 years younger than we are.
Robert Whitcomb (rwhitcomb51@gmail.com), overseer of New England Diary, is a partner in Cambridge Management Group (cmg625.com), a healthcare-sector consultancy, and a fellow of the Pell Center for International Relations and Public Policy.
Robert Whitcomb: Oregon points to better Medicaid
Unsurprisingly, Rhode Island Gov. Gina Raimondo is getting pushback from interest groups against her goal of “reinventing Medicaid’’ – the federal-state program for the poor. The Ocean State’s Medicaid costs are America’s second-highest per enrollee (Alaska is first) and 60 percent higher than the national average.
Many in the nursing-home and hospital industries will fight the governor’s effort to cut costs even if it can be shown that her plan can simultaneously improve care. After all, the current version of Medicaid has been very lucrative for many in those businesses. The Affordable Care Act has brought them even more money.
As we watch her plan unfold, let’s be very skeptical when we hear lobbyists for the healthcare industry and unions asserting that reform would hurt patients. Lobbyists are adept at getting the public to conflate the economic welfare of a sector’s executives, other employees and owners with its customers’. Ambrose Bierce called politics “a strife of interests masquerading as a contest of principles.’’ Often true!
So “nonprofit’’ Lifespan, the state’s largest hospital system, has just hired eight lobbyists to work the General Assembly to defend its interests. (And beware healthcare executives’ citing their businesses’ “nonprofit’’ status. Many of these enterprises take their profit in huge executive compensation.) Some unions are also on the warpath. They worry that reform to reduce the overcharging, waste and duplication pervasive in U.S. health care might reduce the number of jobs.
But economic and demographic reality (including an aging population, widening income inequality and employers’ eliminating their workers’ group insurance) make Medicaid “reinvention’’ mandatory as more patients flood in.
Oregon provides a model of how to do it.
There, in an initiative led by former Gov. John Kitzhaber, M.D., an emergency-room physician, the state has both improved care and controlled costs. It did so by creating 16 regional coordinated-care organizations (CCO’s). The state doesn’t pay for each service performed but gives each CCO a “global budget’’ of Medicaid funds to spend. The emphasis is on having a range of providers work with each other to create holistic treatment plans for patients that include the social determinants of health (such as access to transportation and housing quality) as well as patients’ presenting symptoms.
Oregon’s “fee for value’’ approach rewards providers for meeting performance metrics for quality and efficiency and punishes them for poor outcomes and increased costs.
Oregon CCO’s have great flexibility in spending Medicaid money. For example, they could use it to buy patients air conditioners, which may make it less likely that they’ll show up in the E.R. And Oregon CCO’s pay much attention to how behavioral and mental problems can lead to the more obviously physical manifestations of illness. After all, many in our health-care “system’’ “self-medicate’’ through smoking, drinking, drugs, eating unhealthy food and lack of exercise. You see many of these people again and again in the E.R. –wheezing from smoking and obese.
In Rhode Island, 7 percent of Medicaid beneficiaries account for two-thirds of the spending; many of these “frequent fliers’’ have mental and behavioral health problems best addressed through Oregon-style coordinated care.
Unlike the Oregon approach, the “fee for service’’ system that’s still dominant in U.S. health care encourages hospitals and clinicians to order as many expensive procedures as possible, prescribe the most expensive pills and do other things to maximize profit – and send the bills to the taxpayers, the private insurers and the patients.
But “evidence-based medicine’’ -- as opposed to “reputation-based medicine’’’ -- has helped to show that doing more procedures does not necessarily translate into better outcomes; indeed overtreatment can be lethal. I recommend Dr. H. Gilbert Welch’s book “Less Medicine/More Health’’.
Meanwhile, Oregon points the way:
Among the Oregon Medicaid reform’s achievements: a 5.7 percent drop in inpatient costs; a 21 percent drop in E.R. use (which is always very expensive), and an 11.1 percent drop in maternity costs, largely because of hospitals not performing elective early deliveries before 39 weeks of pregnancy. Thus Oregon officials assert that the state can reach its goal of saving $11 billion in Medicaid costs over 10 years.
Rhode Island can achieve similar successes.
Robert Whitcomb (rwhitcomb51@gmail.com), overseer of New England Diary, is a Providence-based editor and writer and a partner in Cambridge Management Group (cmg625.com), a national healthcare-sector consultancy. He's also a Fellow of the Pell Center for International Relations and Public Policy.
Robert Whitcomb: Still Golden State; Medicaid reform
While driving around Los Angeles’s vastness last week, I kept getting a déjà vu feeling, and not just because I’d been in L.A. before.
My trip reminded me of motoring in the ‘60s, even in the Northeast, with the new and still mostly uncrowded Interstates, cheap gasoline and capacious sense of freedom so that you’d think nothing of jumping into your car, be it a beat-up Chevy or a death-trap VW bug (with the gas tank over your lap), and happily drive for hours to vague destinations.
There’s lots of color in my memories, but also black and white, as in those old Perry Mason and Dragnet shows set in ‘50’s L.A. They and the many films noirs shot in California (e.g., The Big Sleep) recall Somerset Maugham’s calling the French Riviera a “sunny place for shady people.’’
Southern California is preposterous: mountains covered with highly flammable brush and an earthquake-vulnerable desert made to bloom with water diverted/stolen from the Sierra.
And yet, as I GPS’ed from Pasadena and the hip neighborhoods of Silver Lake and Mount Washington across Beverly Hills and out to the farthest points in Malibu, I saw few signs that people were worried.
Lots of water is still being wasted to evaporation via sprinklers and always-uncovered swimming pools – which seem to play more of an aesthetic than an exercise or cooling-off role. A few cars have stickers with which owners laud themselves for saving water by not washing their vehicles, but most seemed recently washed. You view only a few more cactus gardens and a tad fewer fantastically green lawns than two decades ago.
The state is starting to crack down on water waste with big fines, but it can only be the beginning, assuming that the statewide drought continues.
And yet, young people, many fleeing New York’s frigid winters, sweltering summers and astronomical rents are pouring into Los Angeles these days, drawn by the Mediterranean climate, cheaper and more spacious housing and a very contemporary species of decentralized creativity. (Few have read Nathanael West’s dystopian L.A. novel, Day of the Locusts.)
They love Californians’ ingenuity, most famously in recent decades in Silicon Valley but all over the state, as well as its style, much more relaxed than the Northeast’s.
The innovative spirit seems to overcome pessimism and anxiety about drought, general environmental destruction, earthquakes and illegal aliens crossing the border from Mexico.
So California remains the Golden State, the quintessence of the American Dream.
Whether even worse drought, a big quake or a surge in gasoline prices would end car-dependent Los Angeles’s latest boom is unknowable. In any event, mass transit is being expanded. Yes, you can take light rail in the City of Angeles.
This reinvention ethos also characterizes New England, with its ‘er, vigorous climate and rocky soil. Especially in Greater Boston, the capacity to churn out inventions keeps saving our region’s economy, albeit with the occasional recession.
Of course, Southern California has a sunny climate. But we have lots of fresh water, which in the long run is even better. Still, I now think that the Golden State has enough Hollywood and Silicon Valley risk-taking inventiveness to assure its long-term prosperity. Giant solar-powered desalinization plants on the Paramount lot?
xxx
Kudos to Rhode Island Gov. Gina Raimondo for tackling waste in the state Medicaid program. Oregon provides a model of how to do this. Medicare is a much bigger national cost problem for America but harder to control: The old have better lobbyists than the poor.
xxx
Rachel Held Evans’s Washington Post piece, “Want Millennials back in the pews? Stop trying to make church ‘cool’’’ was spot-on. Trying to maintain religion through trendy marketing is doomed. We seek ritual that resists the gyrations of modern commercial culture. We want the permanent and the transcendent to help maintain our sanity.
Even if we don’t believe the theology, we’ll take, say, The Book of Common Prayer over a Facebook “spirituality’’. The faster that technology and the consumer economy go, the more we need the quietly “traditional.’’
Robert Whitcomb (rwhitcomb51@gmail.com), overseer of newenglanddiary.com, is a Providence-based editor and writer, a partner in a health-care-sector consultancy, Cambridge Management Group (cmg625.com) and a Fellow of the Pell Center for International Relations and Public Policy.
Robert Whitcomb: Where we can win; childlessness; water wars
The metastasizing Mideast chaos and violence have shown yet again the limitations of American power there. We’re backing and opposing groups in a fluctuating toxic religious, ethnic, tribal and national stew and frequently contradicting ourselves as we do.
Some neo-cons want us to go in with massive military intervention. We tried that. Now consider that the Sunni fanatics called ISIS use American weaponry captured from the Iraqi “army’’ to attack “Iraq’’ -- whatever that is -- an ally of longtime U.S. enemy Iran, which has joined in the melee against ISIS, even as Sunni Saudi Arabia fights its long-time foe and fellow dictatorship Shiite Iran in Yemen. And in Libya and Syria, the civil wars go on and on in permutations and combinations.
The U.S. must occasionally act quickly in the Mideast to rescue its compatriots and to protect the region’s only real democracy – Israel. But after all this time, we should know that the Mideast has so much confusion, fanaticism and corruption that a heavier U.S. role won’t make things better. The best we can do is to marginalize the region as much as possible, such as by reducing the importance of Mideast fossil fuel by turning more to renewable energy in America and Europe, while, yes, fracking for more gas and oil.
We must focus more on Europe, where a scary situation is much clearer. Our Mideast projects have dangerously diverted resources from countering the far greater threat to our interests posed by Vladimir Putin’s mobster Russian regime.
Now that it has seized Crimea from Ukraine and occupied a big slice of the eastern part of that large democracy, Putin’s fascist police state is firing off yet more threats to “protect’’ ethnic Russians in what he calls “The Russian World’’ (i.e., the old Soviet Empire) from bogus “persecution’’ by the majority population in the Baltic States and Poland -- NATO members and democracies. Latvia is coming under particularly hard Russian pressure now. Hitler used the same strategy against Czechoslovakia with the Sudeten Germans. It’s past time to re-energize NATO to thwart Russian aggressio
xxx
Regarding an April 4 New York Times story headlined “No Kids for Me, Thanks’’:
My mysterious father used to say ruefully that “your friends you can pick, your family you’re stuck with.’’ He had five children.
From observing my childless friends, I’d say that contrary to an old social cliché, they are generally happier than those who have children – so far. A simple reason: They have more money, time and freedom to do what they want.
Arthur Stone, a professor of psychiatry at Stony Brook University who’s co-authored a study comparing childless adults’ happiness and those with kids told CNN: “They {parents} have higher highs. They have more joy in their lives, but also they have more stress and negative emotions as well.’’
CNN said he found “little difference" between “the life satisfaction of parents and people without kids, once other factors -- such as income, education, religion and health -- were factored out.’’ Yes, but how do you ‘’factor out’’ income? Paying for children causes a lot of anxiety.
People tend to be more self-absorbed these days, and so less enthusiastic about sacrificing so much for, say, children. But this presents a problem that some childless Baby Boomers are already experiencing: Who will take care of them when they get really old? If they think that younger friends will feel as compelled to squire them through old age as their children, they’re in Fantasyland.
xxx
The California dream of always-green lawns in McMansion developments in the desert is being revised as drought deepens. (Probably global warming.) The land of Silicon Valley, Cal Tech and Hollywood has more than enough intellectual firepower to address the conservation challenge. (“Dehydrated water – just add water’’?) However, don’t expect many new L.A. Basin golf courses. Californians will see more cactus and less lawn. Meanwhile, places with lots of fresh water -- e.g., New England and the Pacific Northwest – may now be in a better competitive position.
Regarding Golden State water-wars, see the movie “Chinatown’’.
Robert Whitcomb (rwhitcomb51@gmail.com) oversees New England Diary. He's a partner at Cambridge Management Group (cmg625.com), a healthcare-sector consultancy, a Fellow at the Pell Center for International Relations and Public Policy, a former finance editor of the International Herald Tribune, a former editorial-page editor and a vice president at The Providence Journal and a former editor at The Wall Street Journal.
Robert Whitcomb: Republicans bother to vote
‘’The people have spoken … and now they must be punished.’’
-- New York City Mayor Ed Koch’s quip after an election loss
The politicians elected yesterday to new jobs will soon be blamed for doing the same sort of things that their ousted predecessors did as they tried to mate good governance with reality and ambition/ego with idealism.
Distracted and often ignorant citizens, many of whom are usually fleeing reality at a good clip, will demand a perfection from their elected officials that they would never demand of themselves. They will also praise, or more likely blame, the politicians for everything from the weather to the economy’s gyrations. (The first is out of politicians’ control --- unless you factor in the need for us to reduce the amount of carbon dioxide we’re pumping into the air. The second has so many global variables that government’s ability to manage economic cycles remains highly constrained.)
In its existential anxiety, the “the Public’’ will continue to depend on politicians to solve all its problems. Modern electronic media, with their instant ‘’analyses’’ and search for simple, vivid narratives, heighten this dependence and the resulting anger when public/personal problems aren’t immediately fixed.
Our news media (who roughly represent the citizenry’s character flaws) intensify our tendency to pour our hopes and fears into a few people, or even just one (especially the president). Such personalization is easier than trying to understand the details of, say, public policy, economics and history, let alone science.
My sense of the sloth of those who attribute all fault and praise in a big news event to one or very few individuals came together back in 1992, when President George H.W. Bush was in effect blamed for not restoring Dade County, Fla., to its pre-Hurricane Andrew strip-mall glory within 36 hours. Then in 2005, the public blamed his son for the Hurricane Katrina New Orleans mess, although that disaster was inevitable – New Orleans was/is a very corrupt, badly managed city most of which is at sea level or below.
And now some call the complicated (scientifically and otherwise) Ebola situation President Obama’s fault. (That his father was African may inform some of the attacks against him in this….)
Meanwhile, the public takes commands from the media and politicians about how they should feel. If the preponderance of the big (and small) media say that “Americans are pessimistic’’ or ‘’optimistic,’’ then we salute and feel accordingly, whatever the unemployment rate. But not for long, since the conventional-wisdom narrative can be changed overnight and the change “go viral.’’
That’s not to say that politicians’ characters and personalities don’t count – especially in great crises --- e.g., Lincoln in the Civil War or Churchill in the summer of 1940 as Britain stood virtually alone against the Nazi onslaught. But they rarely count nearly as much as we’d like to think they do. Life is far too complicated.
Now we look forward to more gridlock in Washington because the public doesn’t know what it wants (other than more services and lower taxes). It says “government doesn’t work’’ and ensures that it doesn’t by its conflicting and rapidly changing voting -- or, especially in a mid-term election, its nonvotes. The nonvoters are always among the biggest complainers.
Democrats have particularly little excuse for whining this year. A Pew Research Center survey shows that among those who were unlikely to vote last Tuesday, 51 percent favored Democrats and 30 percent the GOP. In this matter, Republicans are harder-working: They summon the energy to take 20 minutes to vote.
xxx
The lack of a direct long-distance rail connection between Boston’s South Station and North Station has always seemed to me ridiculous. Connecting them would make it considerably easier to move between southern and northern New England and further energize passenger rail as demographics (including a huge increase in the number of old people and a new propensity of younger people not to drive) makes public transportation ever more important.
The link should have been made at least a century ago. But the dominant New England railroads of the time – the Boston & Maine (at North Station) and the New Haven (at South Station) -- the city and the state’s couldn’t get it done, as it wasn’t done between New York’s Grand Central Station and Pennsylvania stations.
The Big Dig’s cost overruns haunt efforts to make this link. But rail projects make rich cities even richer by making them more efficient and attractive. The Big Dig made Boston more of a world city. Past gubernatorial foes Michael Dukakis, a Democrat, and Bill Weld, a Republican, recently joined to promote the link. All of New England will benefit if they succeed.
Robert Whitcomb is a Providence-based editor and writer and a partner in Cambridge Management Group (cmg625.com) a healthcare-sector consultancy. A former editorial-page editor for The Providence Journal and a former finance editor of the International Herald Tribune, he's also a Fellow of the Pell Center for International Relations and Public Policy and oversees this site, newenglanddiary.com
Community networks for transforming health care
Video: Marc Pierson, M.D., a senior adviser at Cambridge Management Group West, sets forth a practical program for creating networks of community health workers to help transform American healthcare. Dr. Pierson, a former emergency department physician and hospital executive, has a national reputation for innovation aimed at improving care while reducing per-patient costs. He discusses how real healthcare reform must encompass far more than just the medical sector.
--- Robert Whitcomb (a colleague of Dr. Pierson)
What really is meant by 'patient engagement'?
Cambridge Management Group (cmg625.com) senior adviser <a href="http://www.cfah.org/blog/2014/what-physicians-told-us-about-patient-engagement">Marc Pierson, M.D., had some pithy things </a>to say when he and other experts were recently interviewed by the Center for Advancing Health.
Here are some of the remarks of Dr. Pierson, who is also retired vice president for clinical information and quality for PeaceHealth's St. Joseph Medical Center, Bellingham, Wash.:
<strong> CFAH: ''Here is the CFAH definition of patient engagement: 'Actions people take to support their health and benefit from their health care.' What's missing from this definition? What would you add, subtract or word differently?''</strong> <strong> Dr. Pierson:</strong> ''....Defining {patient} engagement is very much the product of who is doing the defining. If from within health care, then the key question becomes for what or for whom is 'patient' engagement primarily intended to benefit?...I would prefer thinking of 'people' engaged in their health and health care. However, I do like that this definition recognizes that both health and health care require people's active participation...Medical care is not the same as health. Health is much more than the lack of illness...We need to incorporate more perspectives from real people and ask them what they need to become more engaged with their medical conditions, their health, and their well-being.'' <strong>CFAH: ''If a person is engaged in their health and health care, what difference does that make? To whom?''</strong>
<strong>Dr. PIERSON: </strong>"Typically, engagement is defined by health care insiders as paying attention to what you are told to do and being compliant with 'orders.' The current non-system of health care plays into this by being disconnected and difficult for people to understand or navigate....
''Health care offers technology and knowledge but is set up for the people that work inside it, not for its clients' ease, safety, or affordability. Payment for health care is based on professionals managing clients' ill health, not on engaging with people to prevent illness, create well-being, or for self-care of illnesses and chronic conditions.
''People are scared of what they are not allowed to know or understand. They don't want to be more dependent. They don't want to end up going to an emergency room. Their primary relationships are with family, friends, neighborhood, and community — not professional service providers.''
'Triple A' approach to building community health
I chatted a while back with a colleague, James Marcus (Marc) Pierson, M.D., a Cambridge Management Group (cmg625.com) senior adviser. Dr. Pierson — an internist, emergency physician and past vice president of clinical information and quality for PeaceHealth St. Joseph Medical Center, in Bellingham, Wash. — is a major health-care reformer. His leadership in helping to create an integrated and patient-centered health-care system for Whatcom County, Wash., has received national attention.
As a leader of the Pursuing Perfection program in the county, he helped develop the community-based, patient-centric Shared Care health-record system and participated at the board level in the Whatcom Alliance for Healthcare Advancement (WAHA). WAHA helped lead to the recently approved Washington State Health Care Innovation Plan, which has put the power of the state government behind the many ideas arising from Whatcom County’s whole-community and patient-informed perspectives.
He told us that “the county level is the smallest appropriate geographic base for creating a coordinated-care system.’’ Whatcom County was particularly attractive for such efforts because it has attracted a lot of civic-minded and collaboration-minded physicians who “didn’t move here for the money but, among other things, for the natural beauty.’’
Dr. Pierson said that creating an integrated-care model requires first observing how the chaotic traditional “system’’ was or was not working, then trying to understand it and then writing down observations and designing changes. It was crucial to understand the inter-actions of all of the parts of the health-care system, and, crucially, to use patients’ knowledge and opinions – those too-often-neglected elements of health-care reform – in changing the individuals and institutions that serve them.
He cited the “Triple A’’ approach: 1.) research and analyze the needs and desires of the patient population; 2.) understand (clinically and financially) the other parts of the system (doctors, nurses, hospitals, insurers, etc.; 3.) design together one integrated health-care community in which patients’ decisions play the most important part.
With that, he said, we can build a health-care system whose treatment and payment system addresses the ever-changing needs of the whole community. “The quality of the entire system suffers,’’ he said, “when the focus is more on the individual parts and loses sight of the whole community health system. Perfect parts do not make perfect or even good systems. It is the interactions between the parts that must be designed….’’ In any event, the improve-the-parts approach is unsustainable.
Further, Dr. Pierson said, we need to move away from the “extractive financing model’’ of American health care, in which much of the savings from improving a community’s health care leaves the community, making it unavailable for reinvestment. And he touted the idea of setting targets for spending on health within a whole community, citing the success of Jonkoping, Sweden, which set a target of 8.3 percent of the local economy for health care and has had very good outcomes.
He said that his experience in the mid-’80’s as an ER doctor trying to pull together in an ad hoc fashion a variety of specialists to treat a young man badly injured in a motorcycle accident helped get Dr. Pierson thinking about systems and coordination.
This line of focused community building would ultimately lead to his campaign for integrated, community-wide care. Along the way, he made it a point “not to ask anyone to do anything that was against their economic self-interest.’’ And he sought out the “most respected players’’ in the Whatcom health-care community to help him carry out this vision for the county. He's a very practical (and mostly behind-the-scenes) reformer, whose recommendations would be helpful anywhere in the country.
Given the widening income gap in the U.S., we wondered about whether only the rich would have the finest sort of individualized “concierge care’’. Somewhat to our surprise, Dr. Pierson was optimistic that the use of genomic information, personal medical devices and other advances would make “concierge care’’ available to everyone in the fullness of time, aided by the doctors, nurses, social workers and other health-care ‘’navigators’’ who will increasingly see a major part of their jobs as helping to guide patients to the information they need as well as through the system.
It’s all part of his vision to have all of us see “medicine as a part of health and well-being.’’ The whole community, he says, owns its health and well-being and we must design our futures in that context.
-- Robert Whitcomb
Hospital luminary Dr. Daley speaks out on patient safety
Cambridge Management Group Senior Adviser Jennifer Daley, M.D., has held senior executive positions at Tenet Healthcare, Partners Community Healthcare and the University of Massachusetts Memorial Medical Center. She was director of the Center for Health Systems Design and Evaluation at Massachusetts General Hospital/Partners HealthCare, Boston; co-chair and director of research for the National Surgical Quality Improvement Program at the U.S. Department of Veterans Affairs, and vice president and medical director for health-care quality at Beth Israel Deaconess Hospital, Boston. We chatted with her the other day about various things and put it on the Cambridge Management Group site (cmg625.com) but I (Robert Whitcomb) thought that with hospitals so much in the news, it would be good to run it here, too. She focused on hospital-patient safety, on which she is a nationally recognized authority, and referenced the Department of Veterans Affairs situation too.
Dr. Daley said that while there have been heartening “inroads’’ in this area, much more needs to be done to prevent potentially lethal problems, especially avoidable hospital-acquired infections such as bloodstream infections, urinary-tract infections, surgical-wound infections, sepsis and pneumonia acquired from being on a ventilator. We also discussed how inadequate cross-checking by doctors and nurses can lead to perilous drug mistakes, such as with chemotherapy and anti-coagulants.
She said that not enough hospitals follow the protocols needed to dramatically reduce patient-safety issues. “Multidisciplinary groups’’ of physicians and nurses must rally around efforts in hospitals to address these problems. Tools include check-off lists and mandatory frequent repetition of oral questions: e.g., asking doctors “Have you washed your hands’’ and “Are we about to do surgery on the right side?’ ’ and asking patients “What are your allergic to? What’s your date of birth?” (Patient-ID error, of course, can lead to disaster.) And patients and their families, she said, must be further empowered to monitor their treatment and speak up when they sense that something might be wrong. She noted that particularly problematical times are when patients are “handed off’’ to other physicians and nurses during shift changes, when crucial information might fall between the boards.
She observed, meanwhile, that “The Baby Boomers {whose rapidly aging ranks are now flooding into the acute-care system} are more active in monitoring their own care’’ than older people (the “Silent Generation’’), with younger patients (heavy-laden with electronic communication devices useful in communicating with health-care providers) presumably to be even more involved in this ever-more connected world. But while patients, as they are admitted into hospitals, receive printed and oral information about their rights, all too often they are too sick and/or exhausted to fully understand this information. Thus Dr. Daley suggested that patients’ family members and other caregivers be given stronger encouragement to “speak up” and ask questions.
A major problem is that “you often don’t have the bench strength’’ of doctors, nurses and administrators in many hospitals, especially smaller community institutions, compared to academic medical centers, to ensure that more rigorous patient-safety protocols are quickly established, implemented and improved over time.
Dr. Daley said that the “Joint Commission has taken the lead’’ in patient-safety goal setting. That has helped bring along smaller hospitals. The commission, after all, has the sword of certification revocation to get their attention. She also singled out for praise the National Patient Safety Foundation and the American Medical Association.
And, she emphasized, mistakes must be brought out into the open so that providers can understand and prevent their repetition. “Everyone must be transparent about errors.’’
What other powerful weapons do patient-safety advocates have besides moral duty, the fear of license revocation and litigation?
Dr. Daley noted that, payers, most notably the Centers for Medicare and Medicaid Services, are beginning to withhold payments from hospitals with bad outcomes.
Still, the prospect of declining insurance reimbursements because of health-insurance reform and other factors may discourage many hospital senior executives from spending more, mostly on personnel and new, safer technologies, to reduce patient-care errors. They want to protect their institutions’ operating margins.
So, as Dr. Daley said, patient-safety advocates must frequently remind them that the (not very) long-term costs of failing to implement stronger patient-safety measures could be much larger than the short-term expenses of imposing more rigorous patient-safety protocols. After all, hospital-acquired illnesses and injuries do cause life-threatening illnesses and injuries.
Dr. Daley told of how at one hospital, the CFO and his colleagues were shown pictures of infected bed sores that could have been easily prevented by oversight and check-off lists “They quickly changed their minds about the short-term cost being more than worth it.’’
In any event, she noted rather drolly that new medications, technology and health-system organizational changes make it easier to keep patients out of the hospital, offsetting to some extent the expected flood of hospital-bound aging Baby Boomers. The less time that they spend in the hospital, of course, the less likely they are to get infections and other avoidable errors.
Finally, we asked her what she thought of the care-delay-and-coverup scandal at some Department of Veterans Affairs hospitals, with which she is very familiar. (See above.)
“I’m mad,’’ she said, noting “a kind of Civil Service mentality’’ that seems to imply to some incompetent VA managers that “You can’t fire me.’’ She noted that legislation in Congress would help address that problem by making it easier to dismiss problematic senior personnel. And she said the VA system clearly needs many more primary-care doctors – and higher pay for them and those running the hospitals.
Blame Russia for Russian aggression
By ROBERT WHITCOMB (rwhitcomb51@gmail.com)
Some denounce the United States for Russia’s reversion to brutal expansionism into its “Near Abroad” because we encouraged certain Central and Eastern European countries to join the North Atlantic Treaty Organization. The argument is that NATO’s expansion led “Holy Russia” to fear that it was being “encircled.” (A brief look at a map of Eurasia would suggest the imprecision of that word.)
In other words, it’s all our fault. If we had just kept the aforementioned victims of past Russian and Soviet expansionism out of the Western Alliance, Russia wouldn’t have, for example, attacked Georgia and Ukraine. If only everyone had looked into Vladimir Putin’s eyes and decided to trust him.
Really? Russia has had authoritarian or totalitarian expansionist regimes for hundreds of years, with only a few years’ break. How could we have necessarily done anything to end this tradition for all time after the collapse of the Soviet iteration of Russian imperialism? And should we blame Russia’s closest European neighbors for trying to protect themselves from being menaced again by their gigantic and traditionally aggressive neighbor to the east? Russia, an oriental despotism, is the author of current Russian imperialism.
Some of the Blame America rhetoric in the U.S. in the Ukraine crisis can be attributed to U.S. narcissism: the idea that everything that happens in the world is because of us. But Earth is a big, messy place with nations and cultures whose actions stem from deep history and habits that have little or nothing to do with big, self-absorbed, inward-looking America and its 5 percent of the world population. Americans' ignorance about the rest of the planet -- even about Canada! -- is staggering, especially for a "developed nation''.
And we tend to think that “personal diplomacy” and American enthusiasm and friendliness can persuade foreign leaders to be nice. Thus Franklin Roosevelt thought that he could handle “Joe Stalin” and George W. Bush could be pals with another dictator (albeit much milder) Vladimir Putin. They would, our leaders thought, be brought around by our goodwill (real or feigned).
But as a friend used to say when friends told him to “have a nice day”: “I have other plans.”
With the fall of the Soviet Empire, there was wishful thinking that the Russian Empire (of which the Soviet Empire was a version with more globalist aims) would not reappear. But Russian xenophobia, autocracy, anger and aggressiveness never went away.
Other than occupying Russia, as we did Japan and Western Germany after World War II, there wasn’t much we could do to make Russia overcome its worst impulses. (And Germany, and even Japan, had far more experience with parliamentary democracy than Russia had.) The empire ruled from the Kremlin is too big, too old, too culturally reactionary and too insular to be changed quickly into a peaceable and permanent democracy. (Yes, America is insular, too, but in different ways.)
There’s also that old American “can-do” impatience — the idea that every problem is amenable to a quick solution. For some reason, I well remember that two days after Hurricane Andrew blew through Dade County, Fla., in 1992, complaints rose to a chorus that President George H.W. Bush had not yet cleaned up most of the mess. How American!
And of course, we’re all in the centers of our own universes. Consider public speaking, which terrifies many people. We can bring to it extreme self-consciousness. But as a TV colleague once reminded me, most of the people in the audience are not fixated on you the speaker but on their own thoughts, such as on what to have for dinner that night. “And the only thing they might remember about you is the color of the tie you’re wearing.”
We Americans could use a little more fatalism about other countries.
***
James V. Wyman, a retired executive editor of The Providence Journal, was, except for his relentless devotion to getting good stories into the newspaper, the opposite of the hard-bitten newspaper editor portrayed in movies, usually barking out orders to terrified young reporters. Rather he was a kindly, thoughtful and soft-spoken (except for a booming laugh) gentleman with a capacious work ethic and powerful memory.
He died Friday at 90, another loss for the "legacy news media.''
***
My friend and former colleague George Borts died last weekend. He was a model professor — intellectually rigorous, kindly and accessible. As an economist at Brown University for 63 years (!) and as managing editor of the American Economic Review, he brought memorable scholarship and an often entertaining skepticism to his work. And he was a droll expert on the law of unintended consequences.
George wasn’t a cosseted citizen of an ivory tower. He did a lot of consulting for businesses, especially using his huge knowledge of, among other things, transportation and regulatory economics, and wrote widely for a general audience through frequent op-ed pieces. He was the sort of (unpretentious) “public intellectual” that we could use a lot more of.
***
I just read Philip K. Howard’s “The Rule of Nobody: Saving America From Dead Laws and Broken Government.” I urge all citizens to read this mortifying, entertaining and prescriptive book about how our extreme legalism and bureaucracy imperil our future. I’ll write more about the book in this space.
Robert Whitcomb (rwhitcomb51@gmail.com), a former editor of The Providence Journal's editorial pages, is a Providence-based writer and editor, former finance editor of the International Herald Tribune and a partner and senior adviser at Cambridge Management Group (cmg625.com), a consultancy for health systems, and a fellow of the Pell Center for International Relations and Public Policy.
member of.
Dr. Pierson's 'Triple A' for health-care reform
One of my gigs is to help out at a consultancy called Cambridge Management Group, which advises hospitals and other health-care institutions as well as physician groups. I learn the thoughts of some very interesting people. One is nationally known health-care reformer Marc Pierson. Here's the chat/interview I put together the other day and that ran on Cambridge Management 's Web site, cmg625.com.
We chatted the other day with James Marcus (Marc) Pierson, M.D., a Cambridge Management Group senior adviser. Dr. Pierson -- an internist, emergency physician and past vice president of clinical information and quality for PeaceHealth St. Joseph Medical Center, in Bellingham, Wash. -- is a major health-care reformer. His leadership in helping to create an integrated and patient-centered health-care system for Whatcom County, Wash., has received national attention.
As a leader of the Pursuing Perfection program in the county, he helped develop the community-based, patient-centric Shared Care health-record system and participated at the board level in the Whatcom Alliance for Healthcare Advancement (WAHA). <a href="http://whatcomalliance.org/ ">WAHA</a> helped lead to the recently approved Washington State Health Care Innovation Plan, which has put the power of the state government behind the many ideas arising from Whatcom County’s whole-community and patient-informed perspectives.
He told us that “the county level is the smallest appropriate geographic base for creating a coordinated-care system.’’ Whatcom County was particularly attractive for such efforts because it has attracted a lot of civic-minded and collaboration-minded physicians who “didn’t move here for the money but, among other things, for the natural beauty.’’
Dr. Pierson said that creating an integrated-care model requires first observing how the chaotic traditional “system’’ was or was not working, then trying to understand it and then writing down observations and designing changes. It was crucial to understand the inter-actions of all of the parts of the health-care system, and, crucially, to use patients’ knowledge and opinions – those too-often-neglected elements of health-care reform – in changing the individuals and institutions that serve them.
He cited the “Triple A’’ approach: 1.) research and analyze the needs and desires of the patient population; 2.) understand (clinically and financially) the other parts of the system (doctors, nurses, hospitals, insurers, etc.; 3.) design together one integrated health-care community in which patients’ decisions play the most important part.
With that, he said, we can build a health-care system whose treatment and payment system addresses the ever-changing needs of the whole community. “The quality of the entire system suffers,’’ he said, “when the focus is more on the individual parts and loses sight of the whole community health system. Perfect parts do not make perfect or even good systems. It is the interactions between the parts that must be designed….’’ In any event, the improve-the-parts approach is unsustainable.
Further, Dr. Pierson said, we need to move away from the “extractive financing model’’ of American health care, in which much of the savings from improving a community’s health care leaves the community, making it unavailable for reinvestment. And he touted the idea of setting targets for spending on health within a whole community, citing the success of Jonkoping, Sweden, which set a target of 8.3 percent of the local economy for health care and has had very good outcomes.
He said that his experience in the mid-'80’s as an ER doctor trying to pull together in an ad hoc fashion a variety of specialists to treat a young man badly injured in a motorcycle accident helped get Dr. Pierson thinking about systems and coordination.
This line of focused community building would ultimately lead to his campaign for integrated, community-wide care. Along the way, he made it a point “not to ask anyone to do anything that was against their economic self-interest.’’ And he sought out the “most respected players’’ in the Whatcom health-care community to help him carry out this vision for the county. A very practical and behind-the-scenes reformer.
Given the widening income gap in the U.S., we wondered about whether only the rich would have the finest sort of individualized “concierge care’’. Somewhat to our surprise, Dr. Pierson was optimistic that the use of genomic information, personal medical devices and other advances would make “concierge care’’ available to everyone in the fullness of time, aided by the doctors, nurses, social workers and other health-care ‘’navigators’’ who will increasingly see a major part of their jobs as helping to guide patients to the information they need as well as through the system.
It’s all part of his vision to have all of us see “medicine as a part of health and well-being.’’ The whole community, he says, owns its health and well-being and we must design our futures in that context.
Relatively springlike
"Everything Is Relative,'' by MIMO GORDON RILEY, in her current show at the Providence Art Club.
For growers of flowers and vegetables this is a edgy time of year. On the one hand, you want to get the tomatoes, etc., in the ground, on the other, your fear a late frost. Even the more tropical parts of southern New England are vulnerable well into May. This gives a great excuse to put off the work and sleep late on weekends. Growing things is very satisfying but also very tiring, especially when the weeds get going and you can't afford yard crews of undocumented aliens.
By August, a lot of us are longing for the first frost, though that feeling doesn't last long.
You think of summer as a relaxing time but if you're growing things, there's always that pressure to get back to work, albeit outside and not in front of a computer screen. And it's politically correct to grow vegetables because that is seen as harkening back to principles of self-sufficiency, however basically bogus your ambitions in this mission may be since it's much more efficient and usually much cheaper just to buy the products of agribusiness at the supermarket. You can even get "organic'' produce there, if you believe that it actually is. (How can you really find out?)
's m
rwhitcomb51@gmail.com
cmg625.com
newenglanddiary.com
Of factories, Florida and Alzheimer's
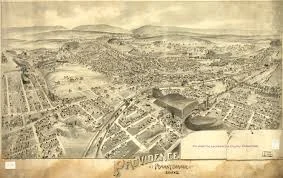
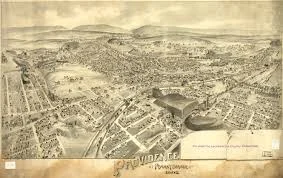
Many citizens wonder what to do with 19 acres of Providence land that have been made available for development by moving Route 195. What a huge opportunity!
The property is in the middle of New England’s second-largest city; alongside the East Coast’s “Main Street” — Route 95 — whose intersection with 195 created one of the East's big crossroads; next to internationally known academic institutions; spectacularly situated at the head of a great bay, and near a large hospital complex. And just down the road is Green Airport, which is being expanded to allow nonstop flights to the West Coast and Western Europe.
What to put on the property? Offices and academic facilities, especially those connected with medically related activities; design businesses (Rhode Island School of Design spinoffs?), restaurants, hotels and stores. But let’s not ignore manufacturing.
This would not be the “dark satanic mills” of yore, emitting thick pollutants into the air and water. Most American manufacturing is much, much cleaner these days. It also employs fewer people, as foreign factories and robotic systems here have taken over much of the work, though the factory workers we have are generally well paid. To make such high-end stuff as pharmaceuticals in plants on the 195 land is just common sense. Consider that the proximity of Routes 195 and 95 and Narragansett Bay’s ports makes shipping manufacturing materials into and finished products out of this part of Providence remarkably easy. And there’s lots of engineering expertise in the region.
And if you think that a factory can’t co-exist attractively with a thickly settled area, consider Genzyme’s plant in the Allston section of Boston.
But the area needs more and better mass transit to serve the neighborhood, whose warren of confusing streets could scare away car-based people. Eventually a couple of trolley lines (real ones, with rails) should run through the newly developed area to connect the old downtown, the medical complex to the south and College Hill. But let development be dense; sociological and other studies associate density with lower crime and higher urban energy. Planners for the land should keep out windswept parking lots.
All in all, the 195 land offers the biggest opportunity to raise the profile and thus the prosperity of Providence since the rivers were moved.
***
We just got back from Naples, Fla., where I worked and we saw relatives in one of the most demure parts of the peninsula. The overloaded airline system makes travel to and from the Sunshine State increasingly difficult. And the urbanization and suburbanization of much of Florida have tattered much of its semi-tropical beauty. Still, the warmth, the greenery and the ease of strolling compared with walking on New England’s icy streets, narrowed by inadequate snowplowing, made it seem paradisiacal. And the quiet was addictive; the sound of wind through the palms and the surf were the main background sounds as I typed in my brother-in-law’s office.
It brought back memories of a quiet, lush Florida from my childhood. I remember the smell of the orange groves, the roadside juice stands and the long stretches of unbuilt-on beach backed only with palmettos and dune grass. My first memory is of an old man throwing bread to pelicans on the beach in Siesta Key, near Sarasota. Later ones include discovering Key lime pie and stone crab, drinking from a coconut and enjoying the best roadside kitsch in America.
Parts of my family had been going to Florida for part of the winter since around World War I. Naturally they complained about its over-development. Of course, they helped start the problem. (However, they never took part in the sort of crazy land speculation immortalized in the Marx Brothers’ 1929 film “The Cocoanuts,” in which Groucho’s character keeps trying to unload swampland on unsuspecting investors. Not much has changed since then!)
When there’s something nice, we overuse it, which is what happened to Florida, especially after air-conditioning, interstate highways and jet travel made getting and staying there so much easier. The Florida that I briefly revisited the other week, just before its high season, evoked in me balmy nostalgia for a time before Florida became a mega-state.
***
Kudos to Cape Cod-based writer/editor/publisher Greg O’Brien, 64, who has been writing (as self-therapy) about Alzheimer’s disease since he was diagnosed with it, in 2009. One of his projects is his book “On Pluto: Inside the Mind of Alzheimer’s.” Then there’s my friend Berna Huebner, whose movie and book, “I Remember Better When I Paint,” describe how her mother, a successful Chicago-based painter, regained some of her skills and energy after she was persuaded to return to painting after Alzheimer’s seemed to doom her to a life of, by turns, agitation and depressed passivity. We’d better be looking for many routes for relief for dementia victims — and their families -- as the number of victims swells in the next two decades.
(In 2010, I wrote a magazine piece about this.)
Robert Whitcomb (rwhitcomb51@gmail.com), a former editor of The Providence Journal's Commentary pages, is a Providence-based writer and editor and the overseer of www.newenglanddiary.com. He is also a director of Cambridge Management Group (cmg625.com).
See news and comment on health-care sector
See the "News'' section of Cambridge Management Group's Web site, www.cmg625.com for news and comment on health care.
Adventures at the Andaz
By ROBERT WHITCOMB (This piece originated at www.cmg625.com).
NEW YORK
I wandered down to the Wired (magazine) Data/Life conference here on Nov. 5-6 on the suggestion of a Cambridge Management Group colleague. There was a lot of interesting stuff that can help people understand where health care, health-care economics and health-care technology are going. And, perhaps especially, where health-care capitalism is going; how fitting that the conference was held at the Andaz Hotel, on Wall Street.
There was remarkably little talk about Obamacare or even about Accountable Care Organizations.
Personal- and population-health data, behavior modification and neat new devices were in the spotlight, and the attendees saw them as considerably more important than Obamacare in the long run. The confab was sponsored by Poland Spring (healthy product, except that oil is used to make its water bottles), IBM (whose Watson computer, with its impressive analytics ability, seems to hold considerable promise for improving health care) and Withings, which makes self-monitoring health devices. Such self-monitoring was a big theme (and marketing play) of the conference.
The first major speaker, Rushika Fernandopulle, M.D., set the stage by noting that great challenges in improving the bad (for the Developed World) U.S. health-care system outcomes and the system’s bankrupting costs include boosting primary care and moving from focusing on acute care to chronic care of diseases, especially such lifestyle-related ones as diabetes, heart disease and certain cancers. As later speakers made clear, new technology and better date are revolutionalizing, by rationalizing, such care already.
Then there was Dr. David Agus, a sort of rock-star (big on TV) cancer doctor and a pioneer in new technologies for personalized health care. The doctor, wearing blue jeans, said it was important to get back to the focus on being able “to die of old age’’ instead of highly preventable diseases. To do this, let’s make far more use of population-health data – think like a climatologist, looking at the earth from above. And let data be your skeptical guide. (Remember when margarine was said to be less bad for you than butter?) And look at the data associated with inactivity -- for instance, that sitting for five hours every day does as much danger to your health as smoking a pack and half a day, he told the crowd.
And, he said, such seemingly small things as going to bed and getting up, and having meals, at the same times of day can be very health-improving. There are real data about this.
Remember, he said, that 50 percent of our health problems are environmental. And read data showing how statins and a baby aspirin cut your risk of heart attack and cancer. (But a later speaker, Dr. David Newman, raised some questions about claims for the routine use of these substances.)
At the same time, Dr. Agus said, some stuff is over-rated or worse, such as taking supplemental doses of Vitamin D. He noted that America spends more on badly or untested supplements than it does on cancer research. Watch the data, with more and more of it available weekly!
While pressing for more data, and pointing to greater patient access to their own personal health data, he also raised the point that constantly watching these data can cause stress…. (Which another new device will monitor?) Which brings up an issue of the whole conference: We’re all supposed to be monitoring ourselves much of the time. Can that get out of control? Will it lead patients to drive doctors and nurses crazy?
It also occurred to me that much of what the conference speakers touted seemed to assume, wrongly, that virtually all Americans can be digital-saavy. In fact, many still don’t have computers and have no idea how to use the Internet. (Going digital is, however, a handy way to lay off more employees and jack up operating profits in the health-care sector and other industries.)
In any case, having much more peer-reviewed data transparency – for medical professionals and patients alike – will be key to improving America’s health outcomes, he suggested.
Then there was David Newman, M.D., of Mt. Sinai Hospital in New York and editor of the very interesting www.TheNNT.com – a data-based site focused on, among other things, on the need to be wary of such panaceas as statins (which, he noted, can give you diabetes). If one has already shown that he or she has heart disease statins can be helpful, but for those who don’t, it can do more harm than good, he said. (The present writer has “severe arterial disease’’ and recently had a triple bypass after many years of taking statins. He’d like more data himself!)
Dr. Newman lauded Affordable Care Act incentives to encourage more skeptical use of stents. He said they’re overprescribed (because lucrative). Indeed, many folks at the conference cited favorably the ACA’s interest in incentives that encourage cost controls that simultaneously improve outcomes. And a more personalized approach to individuals’ risk is needed. We must learn how to better customize treatment.
Beware, he said, of industry-tainted promotion of certain lucrative drugs and procedures.
All in all, he said “Health care has under-treated those without easy access to the system and over-treated those {affluent and/or with insurance} those with it.’’ And what he called “information asymmetry’’ (Iack of transparency) explains much of the medical and economic failures of America’s system.
Ronald DePinho, M.D., president of M.D. Anderson Cancer Center, in Houston, spoke of Anderson’s ambitious plan to sharply reduce some major cancers in the next decade through better use of data (such as using IBM’s Watson artificial intelligence) and public education (e.g., reducing sun exposure amongst children to reduce the likelihood of melanoma later). The idea is to be able to reduce the number of people who go to Anderson and instead be able to diagnose and treat from afar through better data use. Physicians and hospital officials should monitor the Anderson plan carefully. Anderson is, after all, the world’s biggest cancer center.
Martin Blazer, M.D., of New York University, for his part, spent most of his time talking about the beneficial uses of bacteria and the overuse of antibiotics, especially in early childhood. We must, he said, restore our internal “eco-system’’. And we must learn more about our “metabolic pathways.’’ Again, Big Data makes this easier.
Then there were the new medical systems being promoted by some businesspeople. Elizabeth Holmes, of Theranos, talked up her company’s full-service, very patient-friendly laboratory services for drugstores, with only pin pricks needed to get enough blood for full analysis. Theranos has an agreement with Walgreen’s.
Sean Duffy, for his part, talked up Omada Health, which helps patients at risk of diabetes track their behavior through such things as coaching and digital tracking. And Mike Huang talked up Glow, with its mobile app used to predict a woman’s daily fertility cycle, thus, he says, making it easier for couple to conceive. There’s even a financial-assistance program for those who fail to conceive naturally after 10 months!
Life gets more and more intense.
My favorite was Neurotrack, which, as co-founder Elli Kaplan explained, is developing a cognitive test that can detect the earliest neurological effects of Alzheimer’s, thus allowing patients to act to delay its full onset.
Finally, there are devices, discussed in much detail at the conference, with the hope, of course, that venture capitalists there would bite. The conference reminded a little of a car dealership promoting its new models.
Consider David Icke’s company, MC10, which is developing new flexible electronic devices to be worn externally or internally to help diagnoses and therapy. An interesting one is a device to be worn on a football helmet to monitor concussion danger. Then there’s Jawbone, represented by its vice president for software, Jeremiah Robison, like most of the speakers young (and newly rich). It makes wearable devices and audio devices to, among other things, get people to take walks and go to bed to improve their health. (Orwell for president?)
In other words, we and medical professionals will be tracking ourselves every minute. Self-consciousness raised to new levels.
Several speakers suggested that it’s past time to even let the patients, of all people, know what their procedures will cost ahead of time – in the face of secrecy by many health-care institutions and insurance companies, which will fight such transparency all the way because its means they won’t make as much money. Speakers and attendees saw great promise in getting patients to start asking what medical stuff costs. Such questions will change the course of treatment.
The conference made it clear that more transparency was coming with better and better measurement of health-care outcomes. “You can’t improve what you can’t measure,’’ as David Icke of MC10 remarked to the conference.
With wearable health-monitoring devices, much more data and better ways to monitor and analyze it and heightened consumer participation through social media and other new tools, it’s clear that the revolution in health care – and health-care financing -- can only accelerate. It all almost makes the ACA seem inconsequential.
Meanwhile, a bunch of people might become billionaires based on what they learned at the Andaz conference. They’ll be selling stock up the street at the New York Stock Exchange.