Huge UMass med school research building to open in June
Edited from a New England Council report
“The University of Massachusetts Chan Medical School, in Worcester, will finish its new $350 million research facility (above) in June. The 350,000-square-foot center is nine stories high and include a new research space for over 70 principal investigators.
“Multiple departments and programs of the medical school are slated to be relocated to the building, including the Program in Molecular Medicine, the Horae Gene Therapy Center, the Departments of Neurology and Neurobiology, and the school’s new Program in Human Genetics & Evolutionary Biology. The facility is designed to be LEED Gold certified by the U.S. Green Building Council, making the building sustainable and energy efficient.
“‘There is a lot of site work to be done on the quad and around the building,’ said Brian Duffy, senior director of facilities management for capital projects at UMass Chan. ‘The plan is to have the area restored with beautiful green grass by Commencement.”’
Wherever you go, there you are
“Then I was back in it.
The War was on. Outside,
in Worcester, Massachusetts,
were night and slush and cold,
and it was still the fifth
of February, 1918.’’
— From “In the Waiting Room,’’ by Elizabeth Bishop (1911-1979)
Judith Graham: Who will care for elderly patients?
From Kaiser Family Foundation (KFF) Health News
Thirty-five years ago, Jerry Gurwitz was among the first physicians in the United States to be credentialed as a geriatrician — a doctor who specializes in the care of older adults.
“I understood the demographic imperative and the issues facing older patients,” Gurwitz, 67 and chief of geriatric medicine at the University of Massachusetts Chan Medical School, in Worcester, told me. “I felt this field presented tremendous opportunities.”
But today, Gurwitz fears that geriatric medicine is on the decline. Despite the surging older population, there are fewer geriatricians now (just over 7,400) than in 2000 (10,270), he noted in a recent piece in JAMA. (In those two decades, the population 65 and older expanded by more than 60 percent) Research suggests each geriatrician should care for no more than 700 patients; the current ratio of providers to older patients is 1 to 10,000.
What’s more, medical schools aren’t required to teach students about geriatrics, and fewer than half mandate any geriatrics-specific skills training or clinical experience. And the pipeline of doctors who complete a one-year fellowship required for specialization in geriatrics is narrow. Of 411 geriatric fellowship positions available in 2022-23, 30 percent went unfilled.
The implications are stark: Geriatricians will be unable to meet soaring demand for their services as the aged U.S. population swells for decades to come. There are just too few of them. “Sadly, our health system and its workforce are wholly unprepared to deal with an imminent surge of multimorbidity, functional impairment, dementia and frailty,” Gurwitz warned in his JAMA piece.
This is far from a new concern. Fifteen years ago, a report from the National Academies of Sciences, Engineering, and Medicine concluded: “Unless action is taken immediately, the health care workforce will lack the capacity (in both size and ability) to meet the needs of older patients in the future.” According to the American Geriatrics Society, 30,000 geriatricians will be needed by 2030 to care for frail, medically complex seniors.
There’s no possibility that this goal will be met.
What’s hobbled progress? Gurwitz and fellow physicians cite a number of factors: low Medicare reimbursement for services, low earnings compared with other medical specialties, a lack of prestige, and the belief that older patients are unappealing, too difficult, or not worth the effort.
“There’s still tremendous ageism in the health-care system and society,” said geriatrician Gregg Warshaw, a professor at the University of North Carolina School of Medicine.
But this negative perspective isn’t the full story. In some respects, geriatrics has been remarkably successful in disseminating principles and practices meant to improve the care of older adults.
“What we’re really trying to do is broaden the tent and train a health-care workforce where everybody has some degree of geriatrics expertise,” said Michael Harper, board chair of the American Geriatrics Society and a professor of medicine at the University of California-San Francisco.
Among the principles geriatricians have championed: Older adults’ priorities should guide plans for their care. Doctors should consider how treatments will affect seniors’ functioning and independence. Regardless of age, frailty affects how older patients respond to illness and therapies. Interdisciplinary teams are best at meeting older adults’ often complex medical, social, and emotional needs.
Medications need to be reevaluated regularly, and de-prescribing is often warranted. Getting up and around after illness is important to preserve mobility. Nonmedical interventions such as paid help in the home or training for family caregivers are often as important as, or more important than, medical interventions. A holistic understanding of older adults’ physical and social circumstances is essential.
The list of innovations geriatricians have spearheaded is long. A few notable examples:
Hospital-at-home. Seniors often suffer setbacks during hospital stays as they remain in bed, lose sleep, and eat poorly. Under this model, older adults with acute but non-life-threatening illnesses get care at home, managed closely by nurses and doctors. At the end of August, 296 hospitals and 125 health systems — a fraction of the total — in 37 states were authorized to offer hospital-at-home programs.
Age-friendly health systems. Focus on four key priorities (known as the “4Ms”) is key to this wide-ranging effort: safeguarding brain health (mentation), carefully managing medications, preserving or advancing mobility, and attending to what matters most to older adults. More than 3,400 hospitals, nursing homes and urgent care clinics are part of the age-friendly health system movement.
Geriatrics-focused surgery standards. In July 2019, the American College of Surgeons created a program with 32 standards designed to improve the care of older adults. Hobbled by the covid-19 pandemic, it got a slow start, and only five hospitals have received accreditation. But as many as 20 are expected to apply next year, said Thomas Robinson, co-chair of the American Geriatrics Society’s Geriatrics for Specialists Initiative.
Geriatric emergency departments. The bright lights, noise, and harried atmosphere in hospital emergency rooms can disorient older adults. Geriatric emergency departments address this with staffers trained in caring for seniors and a calmer environment. More than 400 geriatric emergency departments have received accreditation from the American College of Emergency Physicians.
New dementia-care models. This summer, the Centers for Medicare & Medicaid Services announced plans to test a new model of care for people with dementia. It builds on programs developed over the past several decades by geriatricians at UCLA, Indiana University, Johns Hopkins University and the University of California at San Francisco.
A new frontier is artificial intelligence, with geriatricians being consulted by entrepreneurs and engineers developing a range of products to help older adults live independently at home. “For me, that is a great opportunity,” said Lisa Walke, chief of geriatric medicine at Penn Medicine, affiliated with the University of Pennsylvania.
The bottom line: After decades of geriatrics-focused research and innovation, “we now have a very good idea of what works to improve care for older adults,” said Harper, of the American Geriatrics Society. The challenge is to build on that and invest significant resources in expanding programs’ reach. Given competing priorities in medical education and practice, there’s no guarantee this will happen.
But it’s where geriatrics and the rest of the health-care system need to go.
Judith Graham is KFF Health News reporter.
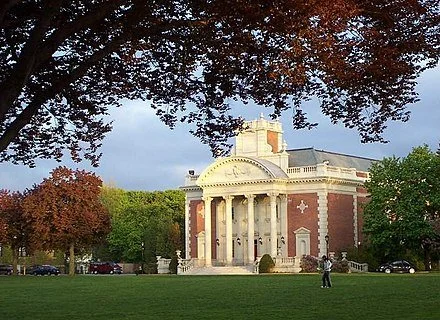
Mapping urban spaces for the public interest
Jonas Clark Hall, the main academic facility for undergraduate students
Edited from a New England Council report
“Clark University, in Worcester, has announced that it will become the first academic institution and founding member of PLACE, a nonprofit data trust committed to mapping urban spaces for the public interest.
“Founded in 2020, PLACE is a technology organization committed to solving the inefficiencies of current urban geo-information data by bridging the gap between and providing data to public and private members. Clark’s Graduate School of Geography (GSG) will support the initiative by using remote sensing to collect high-resolution imagery, which will be open for government and member use. Once surveyed, data from these regions can support research and legislation in a variety of subject areas ranging from housing information to food security.
“‘Clark’s partnership with PLACE will offer our researchers new opportunities to study the processes underlying global change, particularly urbanization, improving our ability to identify solutions to some of our most pressing challenges,’ said Lyndon Estes, associate professor in the GSG.’’
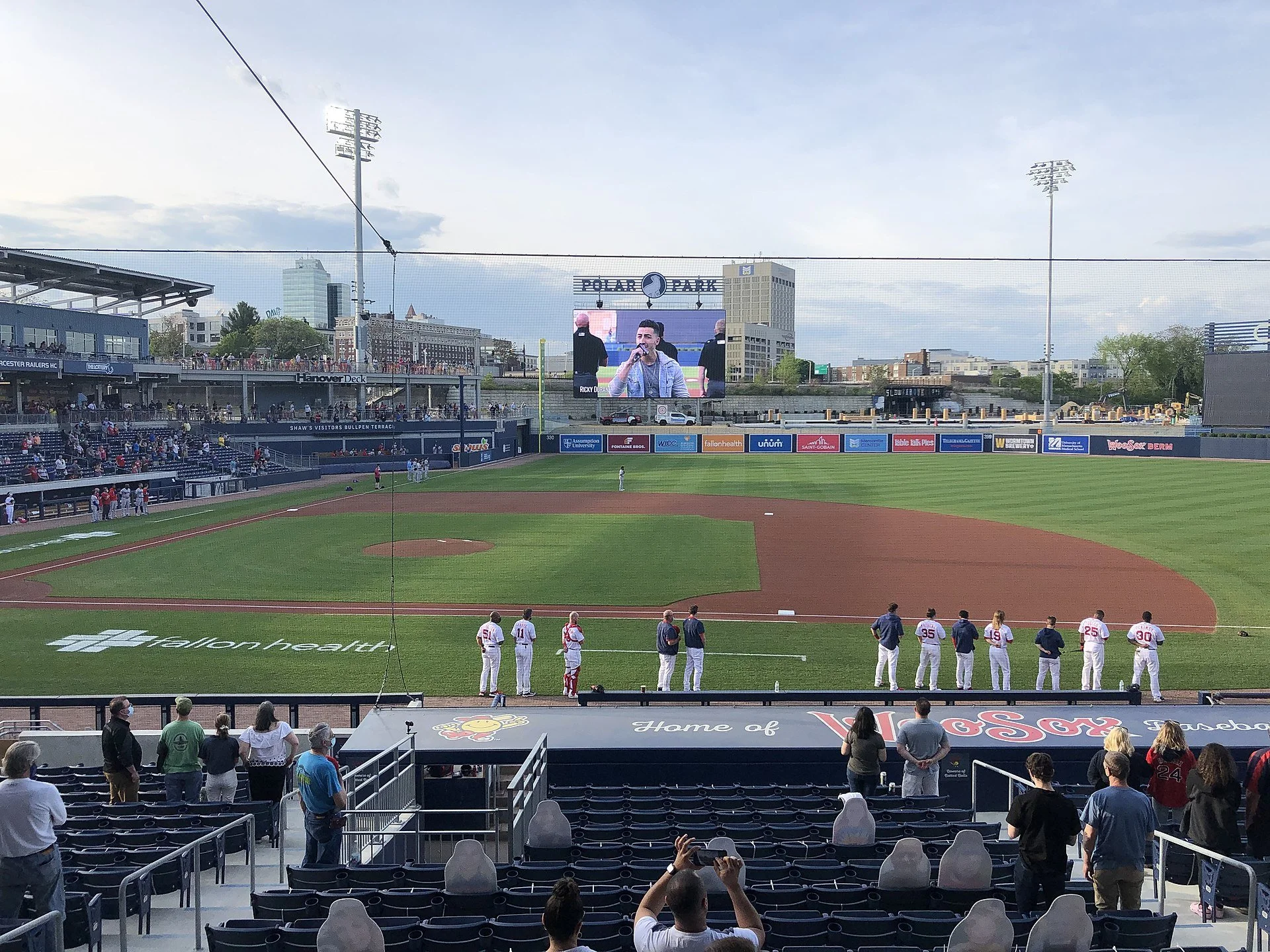
WooSox and summer, etc.
Polar Park, in Worcester
— Photo by MoVaughn123
Adapted from Robert Whitcomb’s “Digital Diary,’’ in GoLocal24.com
On June 11, I drove from Providence to Worcester on Route 146, through old mill towns, to watch the Worcester Red Sox play the Rochester Red Wings at Polar Park. The WooSox won, 5-2, and it was a nice day, with only a little Canadian smoke.
The ballfield is in a gritty and depressing part of the old industrial city, though there’s been some new building in the past couple of years. But I find that looking a few blocks over to the bizarre Union (train) Station’s twin towers, which makes the 1911 structure look like something put up during the Raj, in India, cheers me up, as do the trains running right next to the stadium.
(Don’t feel you have to use the big parking garage next to Polar Park. There’s cheaper and easier surface parking a couple of blocks away.)
The main reason I went to Worcester was to see old friends, who happen to be pals of the WooSox owners. Because of this connection, we watched the game in luxury from a suite with a lounge-like inside area and a porch from which we had a superb view of the field and the stands, though one of my hosts complained that watching a game from a fancy suite at ground level, as was the case with the Pawtucket Red Sox at McCoy Stadium, is more fun. We spent most of our time yakking while sporadically glancing at the action on the field, with cheering the main signal to pay attention.
New professional baseball playing rules, by the way, have blessedly speeded up that action.
There were a little under 9,000 people there -- close to capacity. This is only the stadium’s third year in operation and so probably more than a few in the stands were there out of curiosity to see the glitzy facility. Of course, many baseball fans are still unhappy that this Boston Red Sox affiliate bailed out of Pawtucket. I did see some Rhode Island license plates at Polar Park.
Some economists who are experts in the public financing of such stadiums say that Polar Park will be a long-term drain on the city. Worcester issued $146 million in bonds to build the stadium and owns it. It will take some years to know what the fiscal impact will probably be. The next recession with high unemployment will provide a test; buying a game ticket is, after all, very discretionary. Meanwhile, it has to be said that the WooSox is a very well-run organization.
How much money do WooSox fans from out of town spend in Worcester’s restaurants, etc., outside of Polar Park? Not much, I’d guess. And I doubt that many take in such impressive local cultural venues as the Worcester Art Museum.
Watching baseball, between gossiping with friends and meeting some of their pals for the first time while consuming the likes of lobster rolls or hot dogs (not the latter anymore for me; I avoid eating fellow mammals), popcorn and beer and other goodies is a languid summer pleasure in New England.
As are walking on a beach or along a Vermont stream; letting ice cream and Popsicles drip on your hands; going fishing; eating such vacation artery blockers as fried clams; climbing mountains; sitting on a park bench watching the birds in between desultory looks at a book, and going to country fairs and amusement parks (where you can watch the kids throw up after eating too much candy and then being spun around on a ride).
Summer has certainly changed in our corner of the world in the past five or six decades. One change is the vast expansion of air conditioning. Very few New Englanders had A/C in their homes before around 1970. Movie theaters, restaurants and big stores used to draw many customers simply because they offered cool air.
Summers have generally been getting hotter and longer, and so air conditioning has become increasingly attractive. The tricky thing is that generating the electricity to run the A/C units usually involves burning more fossil fuel, which, in turn, heats up the atmosphere more. Oh, well.
I suspect that home A/C has tended to discourage many people from spending as much time outdoors in the summer as they might have half a century ago – an unhappy change, exacerbated by computer-screen addiction. This probably has played a role in the obesity epidemic. Anyway, we all need more natural light (with sun block on our skin) and exercise. And breezy porches are soothing.
Other notable changes include the building of superhighways to places with great summer allure, most notably in New England -- Cape Cod. This has led to rampant overbuilding there and the erosion of some of the qualities that made The Cape, etc., so beautiful. (I remember the two-way country road with summer farmstands and a piney aroma that led us from Cohasset, Mass., to my grandparents’ house on the Cape in the ‘50s.) And while many folks used to lie for hours in the soporific sunshine, most of us are now aware that we were setting ourselves up for skin cancer.
One improvement is that more people are taking advantage of the fact that summer weather doesn’t end with Labor Day, and can in some years extend into October.
My drive back to Providence from Worcester was thrilling because fewer and fewer drivers these days signal before cutting across lanes. This is particularly menacing in the tangled spaghetti and confusing signage of Worcester’s roads. One guy in an SUV nearly got a bunch of us killed as he swerved across two lanes to get on an exit ramp he belatedly noticed. The best way in and out of Worcester is by helicopter.
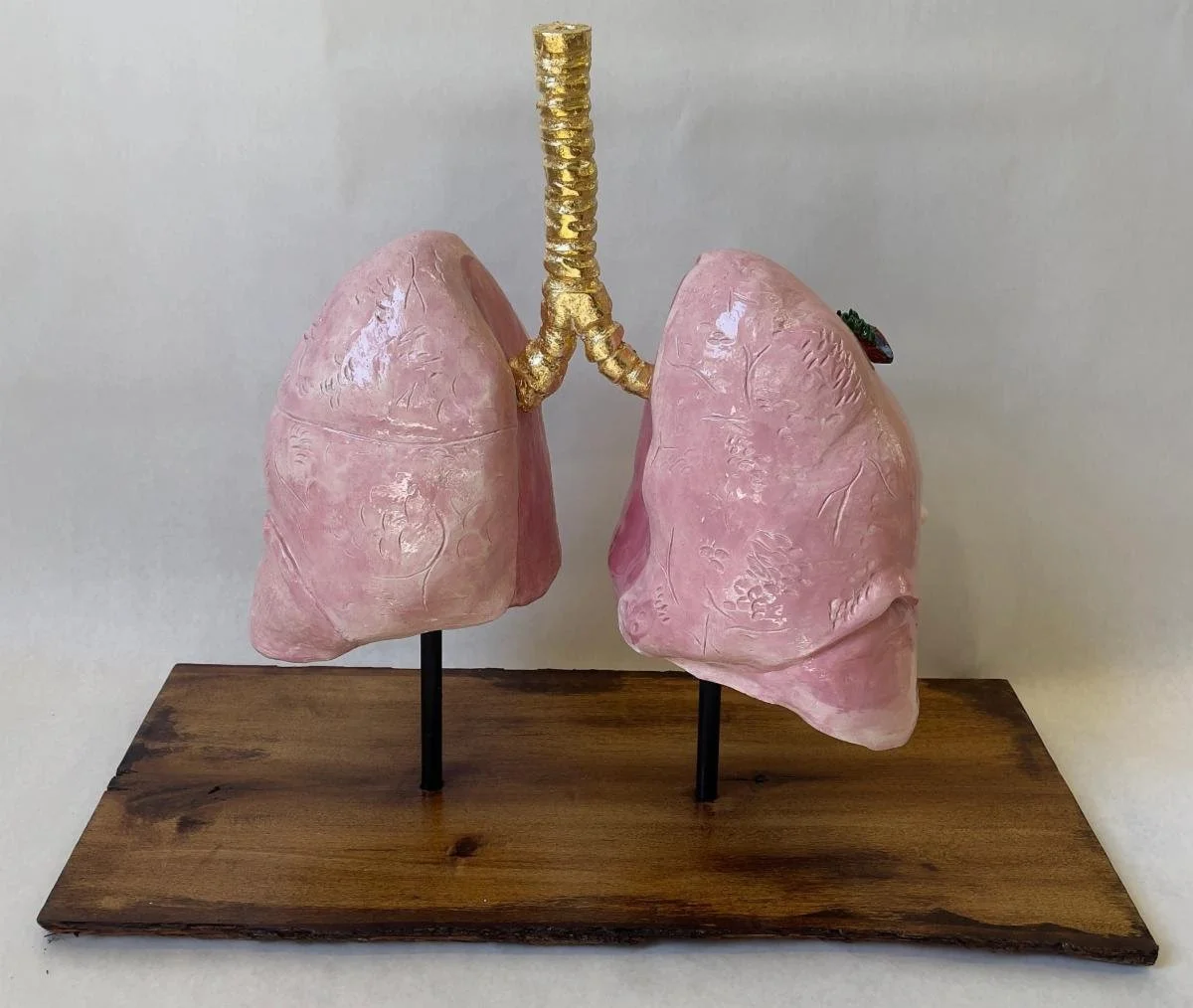
‘Long as you don’t inhale’
“Finding Atmosphere” (ceramic, wood, glaze, gold leaf and wire), by Ethan McGrath, in the show “Essence: 2023 Senior Exhibition,’’ at the Iris and B. Gerald Cantor Art Gallery at the College of the Holy Cross, Worcester, through May 26.
— Photo courtesy of Iris and B. Gerald Cantor Art Gallery
The show brings together the artwork of 13 senior visual-art students — Christian Bachez, Jianing Bai, Brooke Bailey, Aisena Cekrezi, Unique Grimes, Teaken Haggerty, Obiamaka Igwenagu, Ethan McGrath, Kate Nedorostek, Kendra Offermann, Emily Skilton, Noelle Ventura and Olivia Wiatrowsk. The work encompasses a wide range of mediums (and themes) from sculpture, to murals and mixed-media.
xxx
“Pollution,’’ by Tom Lehrer (born 1928), American musician, singer-songwriter, satirist and math professor, including at Harvard, MIT and Wellesley College
If you visit American city,
You will find it very pretty.
Just two things of which you must beware:
Don't drink the water and don't breathe the air!
Pollution, pollution!
They got smog and sewage and mud.
Turn on your tap
And get hot and cold running crud!
See the halibuts and the sturgeons
Being wiped out by detergeons.
Fish gotta swim and birds gotta fly,
But they don't last long if they try.
Pollution, pollution!
You can use the latest toothpaste,
And then rinse your mouth
With industrial waste.
Just go out for a breath of air
And you'll be ready for Medicare.
The city streets are really quite a thrill -
If the hoods don't get you, the monoxide will.
Pollution, pollution!
Wear a gas mask and a veil.
Then you can breathe,
Long as you don't inhale!
Lots of things there that you can drink,
But stay away from the kitchen sink!
The breakfast garbage that you throw into the Bay
They drink at lunch in San Jose.*
So go to the city,
See the crazy people there.
Like lambs to the slaughter,
They're drinking the water
And breathing [cough] the air!
‘Newness on every object’
1850 lithograph
“These towns and cities of New England (many of which would be villages in Old England), are as favourable specimens of rural America, as their people are of rural Americans. The well-trimmed lawns and green meadows of home are not there; and the grass, compared with our ornamental plots and pastures, is rank, and rough, and wild: but delicate slopes of land, gently-swelling hills, wooded valleys, and slender streams, abound. Every little colony of houses has its church and school-house peeping from among the white roofs and shady trees; every house is the whitest of the white; every Venetian blind the greenest of the green; every fine day’s sky the bluest of the blue. A sharp dry wind and a slight frost had so hardened the roads when we alighted at Worcester, that their furrowed tracks were like ridges of granite. There was the usual aspect of newness on every object, of course. All the buildings looked as if they had been built and painted that morning, and could be taken down on Monday with very little trouble.’’
— From American Notes, by Charles Dickens (1812-1870), a travelogue detailing his trip to North America from January to June 1842.
And October alchemy
“Earthly Alchemy’’ (encaustic monotype, ink, pencil, oil pastel on Kitakata), by Worcester-based painter Donna Hamil Talman.
Warner Memorial Theater, at Worcester Academy. Opened in 1932, it was designed by Drew Eberson. The prep school’s famous alumni include computer/lyricist Cole Porter.
Polar Beverages joins national campaign against packaging waste
Orson the Bear, Polar Beverages’ mascot
From The New England Council (newenglandcouncil.com)
BOSTON
New England Council member Polar Beverages, based in Worcester, has joined a national partnership called the Farm Powered Strategic Alliance. The partnership aims to avoid or eliminate food waste, and repurpose what can’t be eliminated into renewable energy via farm-based anaerobic digesters. Polar Beverages is the newest member of the movement which was founded by four food manufacturing companies in 2020.
The two-year alliance is based in Wellesley, Mass., with each member working to do their part to reduce food waste and repurpose non-repurposed materials into renewable energy. The intention of the alliance is to offer a circular approach to reducing emissions of carbon dioxide and serve as a guide for creating a business with a carbon-neutral footprint.
Throughout the years, Polar has transitioned its approach to undertake sustainable manufacturing practices including, upgrading its packaging, cutting water usage and reducing miles driven for product delivery. As a result, Polar has avoided wasting 31 percent of potential wasted packaging material, reduced its water usage by 50,000 gallons a day, and cut miles driven by delivery trucks by 3.5 million over the last three years. The alliance has encouraged Polar to take on another sustainable practice by repurposing wastewater. Now, the wastewater generated from manufacturing will be recycled and turned into anaerobic digesters to be used on six different New England dairy farms.
The executive VP of Polar, Chris Crowley, said, “[w]e couldn’t be more thrilled to join the FPSA and further our commitment to being stewards of the environment.”
The New England Council would like to commend Polar Beverages for its commitment to promoting sustainable practices in New England.
Holy Cross naming science complex after Fauci
Edited from a New England Council (newenglandcouncil.com) report:
“TheCollege of the Holy Cross, in Worcester, is renaming its Integrated Science Complex after its alumni, Dr. Anthony Fauci. Fauci graduated from Holy Cross in 1962 and has since gone on to help guide top federal officials through the coronavirus pandemic. Now, he is serving as chief medical adviser to President Biden.
“Fauci was one of the lead members of the White House Coronavirus Task Force under then- President Donald Trump in the early days of the pandemic. He has served as an adviser to every U.S. president since Ronald Reagan and has been director of the National Institute of Allergy and Infectious Diseases since 1984. The newly named Anthony S. Fauci Integrated Science Complex will officially be dedicated to the physician during his 60th Holy Cross class reunion weekend.
“We are thrilled to celebrate Dr. Fauci in such a public and enduring way,” said Holy Cross President Vincent Rougeau, in a written statement. “It’s fitting that Dr. Fauci’s name will adorn a complex designed to foster integrated learning across multiple academic disciplines – the kind of broad, collaborative and holistic thinking one needs to manage health crises such as HIV/AIDS, Ebola and Zika, or the current COVID-19 pandemic.”
Holy Cross gets $2.5 million for race, gender, social-justice programs with Shakespeare thrown in
At Holy Cross; Fenwick Lawn, with Commencement Porch of Fenwick Hall in the foreground and the chapel beyond.
Edited from a New England Council (newenglandcouncil.com) report.
“The College of the Holy Cross, in Worcester, recently received a $2.5 million gift to be used to establish an endowed chair and lecture series focused on race, gender and social justice.
“The gift comes from Eric Galloway, who graduated from Holy Cross in 1984, and named this lecture series, the Helen M. Whall Lecture Series, an endowed chair position to honor Helen M. Whall, who served as Galloway’s adviser. Whall taught at the college as an English professor from 1976 to her retirement in 2017. History Prof. Rosa Carrasquillo has been selected as the inaugural Helen M. Whall Chair in Race, Gender and Social Justice. The bi-annual lecture series in Whall’s honor will host Shakespearean scholars to come on campus and speak on issues of diversity and equity.
“‘I am honored to acknowledge Helen Whall as an inspiring professor, mentor, and friend to me and other minorities during a sometimes challenging and, ultimately, rewarding time at Holy Cross,’ said Eric Galloway.”
Improving hybrid learning
The Harrington Learning Center on the campus of Quinsigamond Community College, in Worcester.
Edited from a report by The New England Council (newenglandcouncil.com)
“Quinsigamond Community College (QCC) received a $975,000 federal grant to purchase new technology that will improve the hybrid learning experience for its students. This technology, called the HyFlex (hybrid flex) Technology System, will enable instructors to ‘teach students who are taking a course in-person at the same time as students who are taking the course in a remote format,’ and serves to ‘bridge the gap between in-person and online education,’ according to a press release from QCC. The grant provides enough funding to offer HyFlex technology in 25 classrooms.
“Luis Pedraja, president of QCC, said: ‘This technology will be a game-changer for so many students who otherwise would be unable to attend in-person classes.’ She stated that this funding will ‘help facilitate more students to realize a better future through higher education.’’’
Brown study in a nightclub
“Jill at Ralph’s Diner” {restaurant and nightclub in Worcester}, photo by Milford, Mass.-based Anne D. McNevin at the current Attleboro Arts Museum’s members show.
First settled by English colonists in 1662 and incorporated in 1780, Milford became a booming industrial and mining community in the 19th Century, in large part because of a location that includes several rivers for waterpower and other uses, and large quantities of Milford pink granite.
Milford Pink Granite
The Flour and Grain Exchange Building, Boston (1892), built, as were many other large, impressive buildings in the Northeast, with Milford Pink Granite.
Mass. medical schools join to fight racism in health care
Headquarters, in Waltham, of the Massachusetts Medical Society (MMS), the oldest continuously operating state medical association in the United States. Incorporated on Nov. 1, 1781, by an act of the Massachusetts General Court, the MMS is a non-profit organization with more than 25,000 physicians and medical students as members. Its New England Journal of Medicine is among the most prestigious and influential such publications in the world.
From The New England Council (newenglandcouncil.com)
BOSTON
“The University of Massachusetts Medical School, in Worcester, and the Massachusetts Medical Society are joining other medical schools in the state to combat racism in the health-care industry and medicine. The schools released a set of principles targeting racism in medical schools and other health-care organizations.
The schools, including the Boston-based Harvard Medical School, Boston University Medical School and Tufts University Medical School, also in Boston, outlined their long-term goals in a set of four principles. The first principle relates to the need to acknowledge and learn, including from a historical standpoint, as racism in medical practice has had a longstanding presence. The second point calls on institutional leaders to visibly commit to dismantling racism, and the third call for confronting practices and policies devaluing staff and patients of color. The last of the four principles emphasizes a culture of empathy and recognition of the intersectionality of oppression.
“‘It is mission critical for the Medical Society, the DPH (Massachusetts Department of Public Health) and our state’s medical schools to lead in supporting the next generation of physicians and their patients,’ said the Medical Society’s president, Dr. Carole Allen. ‘This document outlines important steps to address systemic racism as it manifests in health care.”’
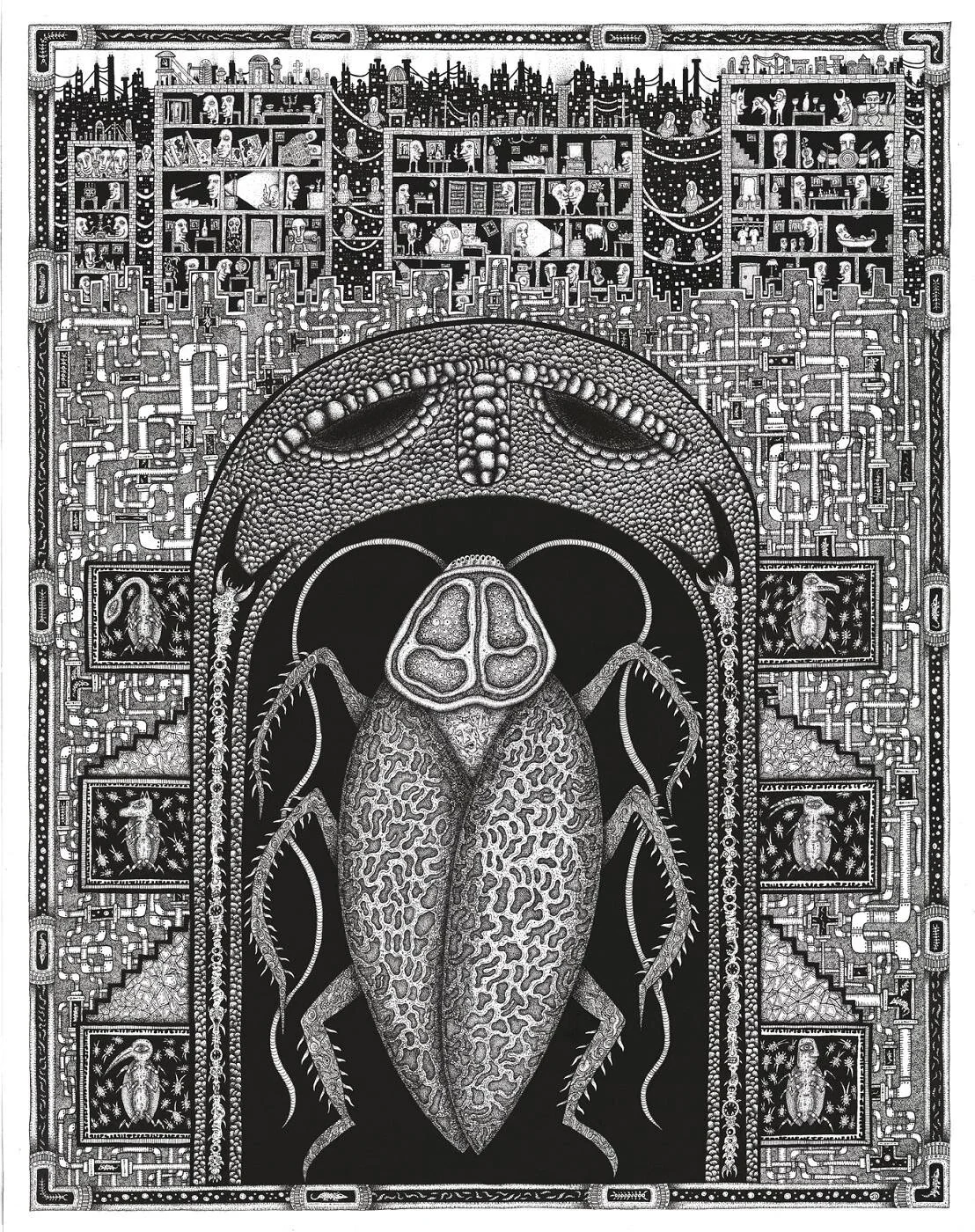
Monarch of metroland
“Citadel of the Roach Queen” (dip pen and India ink), by Worcester-based James Dye, in the New England XI, a regional juried exhibition, at Galatea Fine Art, Boston, Aug. 6-29. Mr. Dye grew up in Holden, near Worcester.
Holden Center
May Worcester's big baseball gamble pay off
Rendition of Polar Park
From Robert Whitcomb’s “Digital Diary,’’ in GoLocal24.com
The new, $159.5 million Polar Park project, in Worcester, looks lovely, as well it should at that price. Worcester, through borrowing, is paying $88.2 million, the Worcester Red Sox $60.6 million and the state and Feds $10.7 million, at least according to a Feb. 4 Worcester Business Journal report.
Will Polar Park pay for itself in bigger local business revenues and payrolls and such related public benefits as more municipal-property-tax revenue? Generally, publicly financed sports stadiums don’t pay for themselves, at least in measurable monetary benefits for the taxpayers, though of course they can be very lucrative for the team owners. And there can be psychic benefits for some locals from the pride in having a (hopefully) successful team to rally around and an often jolly place to gather.
In the case of Worcester, I have some doubts on whether, after a year or two of people drawn by curiosity to the new ballpark, the WooSox can lure the number of long-term gamegoers they hope for.
While Worcester was very narrowly the second-largest city in New England in the 2010 Census, with 181,045 people, compared to Providence’s 178,042, its metro area had only 923,672 people, compared to Greater Providence’s 1.6 million. Providence proper’s area is only 20.58 square miles, compared with Worcester’ 38.41.
Those numbers seemingly would have made it much more sensical to keep the Pawtucket Red Sox going, even with less than the substantial taxpayer help that the organization had been offered in the Ocean State. Further, Providence/Pawtucket is on the main street of the East Coast and Worcester is more off to the side.
Well, que sera, sera. Now that Polar Park is up, I wish the WooSox all the best and plan a trip there soon to check it out. While I have little interest in such things as baseball statistics (real baseball fans are obsessed with such data) and don’t much follow the ups-and-downs of current stars, I do love the setting, sights and sounds of baseball: The slope of the stands; the smell of very green grass and of hot dogs and beer; the cheers (and boos); the crack of the ball against the bat; the tacky organ music; the alternations of relative immobility and explosive activity; the manic announcers, and the seventh inning stretch.
As for folks living in and around Worcester, perhaps it will become one of those “third places,’’ such as restaurants, coffee shops, gyms and even some bookstores, where locals go to hang out with their neighbors on a regular basis. We may know within a couple of years. Maybe it will become as beloved a local institution (for many) as Clark University, the College of the Holy Cross, Worcester Polytechnic Institute and the Worcester Museum of Art, and as the PawSox were for so many years in Greater Providence. Maybe.
Walk into 'collective memory'
“Memory Gates,’’ by Syrian-born Kevork Mourad, at the Cantor Art Gallery of the College of the Holy Cross, Worcester, through April 11.
The gallery says:
“Using his signature style of spontaneous drawing and printmaking techniques, artist Kevork Mourad created the site-specific immersive installation ‘‘Memory Gates ‘‘ during a residency at the Cantor Art Gallery in February. The work, a series of doors and passageways that visitors can pass through, explores themes of cultural plurality and collective memory. Co-sponsored by the Cantor Art Gallery and Arts Transcending Borders.’’
Anthony S. Fauci: What I learned at Holy Cross
At Holy Cross: O'Kane Hall and clock tower. The 175-acre campus has an irregular layout on a steep hill named Mount Saint James, which offers a panoramic view of Worcester.
“Knowledge goes hand-in-hand with truth — something I learned with a bit of tough love from my Jesuit education at Regis High School in New York and then at the College of the Holy Cross, in Worcester.’’
— Anthony S. Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases since 1984
Charlotte Huff: In COVID crisis, 'unattended moral injury' to health-care workers
St. Vincent Hospital in Worcester
For Christina Nester, the pandemic lull in Massachusetts lasted about three months through summer into early fall. In late June, St. Vincent Hospital had resumed elective surgeries, and the unit the 48-year-old nurse works on switched back from taking care of only COVID-19 patients to its pre-pandemic roster of patients recovering from gallbladder operations, mastectomies and other surgeries.
That is, until October, when patients with coronavirus infections began to reappear on the unit and, with them, the fear of many more to come. “It’s paralyzing, I’m not going to lie,” said Nester, who’s worked at the Worcester hospital for nearly two decades. “My little clan of nurses that I work with, we panicked when it started to uptick here.”
Adding to that stress is that nurses are caught betwixt caring for the bedside needs of their patients and implementing policies set by others, such as physician-ordered treatment plans and strict hospital rules to ward off the coronavirus. The push-pull of those forces, amid a fight against a deadly disease, is straining this vital backbone of health providers nationwide, and that could accumulate to unsustainable levels if the virus’s surge is not contained this winter, advocates and researchers warn.
Nurses spend the most sustained time with a patient of any clinician, and these days patients are often very fearful and isolated, said Cynda Rushton, a registered nurse and bioethicist at Johns Hopkins University, in Baltimore.
“They have become, in some ways, a kind of emotional surrogate for family members who can’t be there, to support and advise and offer a human touch,” Rushton said. “They have witnessed incredible amounts of suffering and death. That, I think, also weighs really heavily on nurses.”
A study published this fall in the journal General Hospital Psychiatry found that 64 percent of clinicians working as nurses, nurse practitioners or physician assistants at a New York City hospital screened positively for acute distress, 53 percent for depressive symptoms and 40 percent for anxiety — all higher rates than found among physicians screened.
Researchers are concerned that nurses working in a rapidly changing crisis like the pandemic — with problems ranging from staff shortages that curtail their time with patients to enforcing visitation policies that upset families — can develop a psychological response called “moral injury.” That injury occurs, they say, when nurses feel stymied by their inability to provide the level of care they believe patients require.
Dr. Wendy Dean, co-founder of Moral Injury of Healthcare, a nonprofit organization based in Carlisle, Pa., said, “Probably the biggest driver of burnout is unrecognized unattended moral injury.”
In parts of the country over the summer, nurses got some mental-health respite when cases declined, Dean said.
“Not enough to really process it all,” she said. “I think that’s a process that will take several years. And it’s probably going to be extended because the pandemic itself is extended.”
Before the pandemic hit her Massachusetts hospital “like a forest fire” in March, Nester had rarely seen a patient die, other than someone in the final days of a disease like cancer.
Suddenly she was involved with frequent transfers of patients to the intensive-care unit when they couldn’t breathe. She recounts stories, imprinted on her memory: The woman in her 80s who didn’t even seem ill on the day she was hospitalized, who Nester helped transport to the morgue less than a week later. The husband and wife who were sick in the intensive care unit, while the adult daughter fought the virus on Nester’s unit.
“Then both parents died, and the daughter died,” Nester said. “There’s not really words for it.”
During these gut-wrenching shifts, nurses can sometimes become separated from their emotional support system — one another, said Rushton, who has written a book about preventing moral injury among health- care providers. To better handle the influx, some nurses who typically work in noncritical care areas have been moved to care for seriously ill patients. That forces them to not only adjust to a new type of nursing, but also disrupts an often-well-honed working rhythm and camaraderie with their regular nursing co-workers, she said.
At St. Vincent Hospital, the nurses on Nester’s unit were told one March day that the primarily post-surgical unit was being converted to a COVID unit. Nester tried to squelch fears for her own safety while comforting her COVID-19 patients, who were often elderly, terrified and sometimes hard of hearing, making it difficult to communicate through layers of masks.
“You’re trying to yell through all of these barriers and try to show them with your eyes that you’re here and you’re not going to leave them and will take care of them,” she said. “But yet you’re panicking inside completely that you’re going to get this disease and you’re going to be the one in the bed or a family member that you love, take it home to them.”
When asked if hospital leaders had seen signs of strain among the nursing staff or were concerned about their resilience headed into the winter months, a St. Vincent spokesperson wrote in a brief statement that during the pandemic “we have prioritized the safety and well-being of our staff, and we remain focused on that.”
Nationally, the viral risk to clinicians has been well documented. From March 1 through May 31, 6 percent of adults hospitalized were health-care workers, one-third of them in nursing-related occupations, according to data published last month by the Centers for Disease Control and Prevention.
As cases mount in the winter months, moral injury researcher Dean said, “nurses are going to do the calculation and say, ‘This risk isn’t worth it.’”
Juliano Innocenti, a traveling nurse working in the San Francisco area, decided to take off for a few months and will focus on wrapping up his nurse practitioner degree instead. Since April, he’s been seeing a therapist “to navigate my powerlessness in all of this.”
Innocenti, 41, has not been on the front lines in a hospital battling COVID-19, but he still feels the stress because he has been treating the public at an outpatient dialysis clinic and a psychiatric hospital and seen administrative problems generated by the crisis. He pointed to issues such as inadequate personal protective equipment.
Innocenti said he was concerned about “the lack of planning and just blatant disregard for the basic safety of patients and staff.” Profit motives too often drive decisions, he suggested. “That’s what I’m taking a break from.”
Building Resiliency
As cases surge again, hospital leaders need to think bigger than employee-assistance programs to backstop their already depleted ranks of nurses, Dean said. Along with plenty of protective equipment, that includes helping them with everything from groceries to transportation, she said. Overstaff a bit, she suggested, so nurses can take a day off when they hit an emotional cliff.
The American Nurses Association, the American Association of Critical-Care Nurses (AACN) and several other nursing groups have compiled online resources with links to mental health programs as well as tips for getting through each pandemic workday.
Kiersten Henry, an AACN board member and nurse practitioner in the intensive care unit at MedStar Montgomery Medical Center, in Olney, Md., said that the nurses and other clinicians there have started to gather for a quick huddle at the end of difficult shifts. Along with talking about what happened, they share several good things that also occurred that day.
“It doesn’t mean that you’re not taking it home with you,” Henry said, “but you’re actually verbally processing it to your peers.”
When cases reached their highest point of the spring in Massachusetts, Nester said there were some days she didn’t want to return.
“But you know that your friends are there,” she said. “And the only ones that really truly understand what’s going on are your co-workers. How can you leave them?”
Charlotte Huff is a Kaiser Health News reporter.
UMass Memorial plans Worcester field hospital for COVID-19 patients
The DCU Center (originally Centrum) is an indoor arena and convention center complex in downtown Worcester.
Here’s The New England Council’s (newenglandcouncil.com) latest roundup of COVID-19 news in our region:
* ‘‘UMass Memorial Health Care has laid plans for a field hospital in the DCU Center in Worcester. (DCU stands for Digital Federal Credit Union.) The field hospital was decommissioned last spring; however, UMass Memorial has since been preparing to open the site once again in anticipation of another surge in COVID-19 related hospitalizations. Read more here.’’
* ‘‘ Mass General Brigham and Beth Israel Lahey Health are reporting that their hospitals are better prepared for a second COVID-19 wave. Hospital officials are in communication to balance COVID-19 patients across multiple sites in the Greater Boston area if the need arises. Read more here. ‘‘
* ”The American Hospital Association has produced a podcast providing useful information on patient wellness, preventing chronic diseases, and prioritizing quality and patient safety during the COVID-19 pandemic. Read more here. ‘‘
* ’’ (Boston-based) Harbor Health Services has partnered with instaED Paramedics to provide elders who participate in their Elder Service Plan (ESP) with at-home urgent care. The program will allow participants to receive treatments normally provided in the emergency room while safe at home. Read more here.’’