Harris Meyer: Mass. pushing back against at pricey hospital group’s empire building
Pen and wash drawing by the malacologist Pierre de Montfort, 1801.
Front entrance of Massachusetts General Hospital.
A Massachusetts health-cost watchdog agency and a broad coalition including consumers, health systems, and insurers helped block the state’s largest — and most expensive — hospital system in April from expanding into the Boston suburbs.
Advocates for more affordable care hope that the decision by regulators to hold Mass General Brigham accountable for its high costs will usher in a new era of aggressive action to rein in hospital expansions that drive up spending. Their next target is a proposed $435 million expansion by Boston Children’s Hospital.
Other states, including California and Oregon, are paying close attention, eyeing ways to emulate Massachusetts’s decade-old system of monitoring health-care costs, setting a benchmark spending rate, and holding hospitals and other providers responsible for exceeding their target.
The Massachusetts Health Policy Commission examines hospital-specific data and recommends to the state Department of Public Health whether to approve mergers and expansions. The commission also can require providers and insurers to develop a plan to reduce costs, as it’s doing with MGB.
“The system is working in Massachusetts,” said Maureen Hensley-Quinn, a senior program director at the National Academy for State Health Policy, who stressed the importance of the state’s robust data-gathering and analysis program. “The focus on providing transparency around health costs has been really helpful. That’s what all states want to do. I don’t know if other states will adopt the Massachusetts model. But we’re hearing increased interest.”
With its many teaching hospitals, Massachusetts historically has been among the states with the highest per capita health-care costs, though its spending has moderated in recent years as state officials have taken aim at the issue.
On April 1, MGB, an 11-hospital system that includes the famed Massachusetts General Hospital, unexpectedly withdrew its proposal for a $223.7 million outpatient-care expansion in the suburbs after being told by state officials it wouldn’t be approved.
That expansion would have increased annual spending for commercially insured residents by as much as $28 million, driving up insurance premiums and shifting patients away from lower-priced competitors, according to the commission.
This marked the first time in decades that the state health department used its authority to block a hospital expansion because it undercut the state’s goals to control health costs.
Other parts of MGB’s $2.3 billion expansion plan also met resistance.
The health department staff recommended approving MGB’s proposal to build a 482-bed tower at its flagship Massachusetts General Hospital and a 78-bed addition at Brigham and Women’s Faulkner Hospital. But they urged rejecting a request for 94 additional beds at MGH.
The department’s Public Health Council, whose members are mostly appointed by the governor, is scheduled to vote on those recommendations May 4.
The health policy commission, which works independently of the public health department but provides advice, has also required MGB to submit an 18-month cost-control plan by May 16, because its prices and spending growth have far exceeded those of other hospital systems. That was a major reason the growth in state health spending hit 4.3 percent in 2019, exceeding the commission’s target of 3.1%.
This is the first time a state agency in Massachusetts or anywhere else in the country has ordered a hospital to develop a plan to control its costs, Hensley-Quinn said.
MGB’s $2.3 billion expansion plan and its refusal to acknowledge its high prices and their impact on the state’s health costs have united a usually fractious set of stakeholders, including competing hospitals, insurers, employers, labor unions and regulators. They also were angered by MGB’s lavish advertising campaign touting the consumer benefits of the expansion.
Their fight was bolstered by a report last year from state Atty. Gen. Maura Healey that found that the suburban outpatient expansion would increase MGB annual profits by $385 million. The nonprofit MGB reported $442 million in operating income in 2021.
The Massachusetts Association of Health Plans opposed the MGB outpatient expansion.
The well-funded coalition warned that the expansion would severely hurt local hospitals and other providers, including causing job losses. The consumer group Health Care for All predicted the shift of patients to the more expensive MGB sites would lead to higher insurance premiums for individuals and businesses.
“Having all that opposition made it pretty easy for [the Department of Public Health] to do the right thing for consumers and cost containment,” said Lora Pellegrini, CEO of the health plan association.
Republican Gov. Charlie Baker, who has made health-care cost reduction a priority and who leaves office next January after eight years, didn’t want to see the erosion of the state’s pioneering system of global spending targets, she said.
“What would it say for the governor’s legacy if he allowed this massive expansion?” she added. “That would render our whole cost-containment structure meaningless.”
MGB declined to comment.
Massachusetts’s aggressive action examining and blocking a hospital expansion comes after many states have moved in the opposite direction. In the 1980s, most states required hospitals to get state permission for major projects under “certificate of need” laws. But many states have loosened or abandoned those laws, which critics say stymied competition and failed to control costs.
The Trump administration recommended that states repeal those laws and leave hospital-expansion projects up to the free market.
But there are signs the tide is turning back to more regulation of hospital building.
Several states have created or are considering creating commissions similar to the one in Massachusetts with the authority and tools to analyze the market impact of expansions and mergers. Oregon, for example, recently passed a law empowering a state agency to review health care mergers and acquisitions to ensure they maintain access to affordable care.
Despite the defeat of MGB’s outpatient expansion, Massachusetts House Speaker Ron Mariano, a Democrat, said the state’s cost-control model needs strengthening to prevent hospitals from making an end run around it. A bill he backed that passed the House would give the commission and the attorney general’s office a bigger role in evaluating the cost impact of expansions. The Senate hasn’t taken up the bill.
“Hospital expansion is the biggest driver in the whole medical expense kettle,” he said.
Meanwhile, cost-control advocates are eager to see how MGB proposes to control its spending, and how the Health Policy Commission responds.
“Unless MGB somehow agrees to limit increases in its supranormal pricing, like a five-year price freeze across the system, I don’t know that the [plan] will accomplish anything,” said Dr. Paul Hattis, a former commission member.
Hattis and others are also waiting to see how the state rules on a bid by Boston Children’s Hospital, another high-priced provider, to build new outpatient facilities in the suburbs.
“For those of us on the affordability side, it’s like the sheriffs rediscovered their badge and realized they really could say no,” he said. “That’s a message to other states that they also should constrain their larger provider systems, and to the systems that they can no longer do whatever they please.”
Harris Meyer is a Kaiser Health News reporter.
Melissa Bailey: In Mass. and elsewhere, climate change hurts patients’ health
Mount Auburn Hospital's first building, the Parsons Building, built 1886. Patients had to be moved in the Cambridge hospital in 2019 because of a heat wave.
BOSTON
A 4-year-old girl was rushed to the emergency room three times in one week for asthma attacks.
An elderly man, who’d been holed up in a top-floor apartment with no air conditioning during a heat wave, showed up at a hospital with a temperature of 106 degrees.
A 27-year-old man arrived in the ER with trouble breathing ― and learned he had end-stage kidney disease, linked to his time as a sugar-cane farmer in the sweltering fields of El Salvador.
These patients, whose cases were recounted by doctors, all arrived at Boston-area hospitals in recent years. While the coronavirus pandemic is at the forefront of doctor-patient conversations these days, there’s another factor continuing to shape patients’ health: climate change.
Global warming is often associated with dramatic effects such as hurricanes, fires and floods, but patients’ health issues represent the subtler ways that climate change is showing up in the exam room, according to the physicians who treated them.
Dr. Renee Salas, an emergency physician at Massachusetts General Hospital, in Boston, said that she was working a night shift when the 4-year-old arrived the third time, struggling to breathe. The girl’s mother felt helpless that she couldn’t protect her daughter, whose condition was so severe that she had to be admitted to the hospital, Salas recalled.
She found time to talk with the patient’s mother about the larger factors at play: The girl’s asthma appeared to be triggered by a high pollen count that week. And pollen levels are rising in general because of higher levels of carbon dioxide, which she explained is linked to human-caused climate change.
Salas, a national expert on climate change and health, is a driving force behind an initiative to spur clinicians and hospitals to take a more active role in responding to climate change. The effort launched in Boston last February, and organizers aim to spread it to seven U.S. cities and Australia over the next year and a half.
Although there is scientific consensus on a mounting climate crisis, some people reject the idea that rising temperatures are linked to human activity. The controversy can make doctors hesitant to bring it up.
Even at the climate-change discussion in Boston, one panelist suggested the topic may be too political for the exam room. Dr. Nicholas Hill, head of the Pulmonary, Critical Care and Sleep Division at Tufts Medical Center of Medicine, in Boston, recalled treating a “cute little old lady” in her 80s who likes Fox News, a favorite of climate-change doubters. With someone like her, talking about climate change may hurt the doctor-patient relationship, he suggested. “How far do you go in advocating with patients?”
Doctors and nurses are well suited to influence public opinion because the public considers them “trusted messengers,” said Dr. Aaron Bernstein, who co-organized the Boston event and co-directs the Center for Climate, Health, and the Global Environment at Harvard’s school of public health. People have confidence they will provide reliable information when they make highly personal and even life-or-death decisions.
Bernstein and others are urging clinicians to exert their influence by contacting elected officials, serving as expert witnesses, attending public protests and reducing their hospital’s carbon emissions. They’re also encouraging them to raise the topic with patients.
Dr. Mary Rice, a pulmonologist who researches air quality at Beth-Israel Deaconess Medical Center here, recognized that in a 20-minute clinic visit, doctors don’t have much time to spare.
But “I think we should be talking to our patients about this,” she said. “Just inserting that sentence, that one of the reasons your allergies are getting worse is that the allergy season is worse than it used to be, and that’s because of climate change.”
Salas, who has been a doctor for seven years, said she had little awareness of the topic until she heard climate change described as the “greatest public health emergency of our time” during a 2013 conference.
“I was dumbfounded about why I hadn’t heard of this, climate change harming health,” she said. “I clearly saw this is going to make my job harder” in emergency medicine.
Now, Salas said, she sees ample evidence of climate change in the exam room. After Hurricane Maria devastated Puerto Rico, for instance, a woman seeking refuge in Boston showed up with a bag of empty pill bottles and thrust it at Salas, asking for refills, she recalled. The patient hadn’t had her medications replenished for weeks because of the storm, whose destructive power was likely intensified by climate change, according to scientists.
Climate change presents many threats across the country, Salas noted: Heat stress can exacerbate mental illness, prompt more aggression and violence, and hurt pregnancy outcomes. Air pollution worsens respiratory problems. High temperatures can weaken the effectiveness of medications such as albuterol inhalers and EpiPens.
The delivery of health care is also being disrupted. Disasters like Hurricane Maria have caused shortages in basic medical supplies. Last November, nearly 250 California hospitals lost power in planned outages to prevent wildfires. Natural disasters can interrupt the treatment of cancer, leading to earlier death.
Even a short heat wave can upend routine care: On a hot day in 2019, for instance, power failed at Mount Auburn Hospital, in Cambridge, Mass., and firefighters had to move patients down from the top floor because it was too hot, Salas said.
Other effects of climate change vary by region. Salas and others urged clinicians to look out for unexpected conditions, such as Lyme disease and West Nile virus, that are spreading to new territory as temperatures rise.
In California, where wildfires have become a fact of life, researchers are scrambling to document the ways smoke inhalation is affecting patients’ health, including higher rates of acute bronchitis, pneumonia, heart attacks, strokes, irregular heartbeats and premature births.
Researchers have shown that heavy exposure to wildfire smoke can change the DNA of immune cells, but they’re uncertain whether that will have a long-term impact, said Dr. Mary Prunicki, director of air pollution and health research at Stanford University’s center for allergy and asthma research.
“It causes a lot of anxiety,” Prunicki said. “Everyone feels helpless because we simply don’t know — we’re not able to give concrete facts back to the patient.”
In Denver, Dr. Jay Lemery, a professor of emergency medicine at the University of Colorado School of Medicine, said he’s seeing how people with chronic illnesses like diabetes and chronic obstructive pulmonary disease suffer more with extreme heat.
There’s no medical code for “hottest day of the year,” Lemery said, “but we see it; it’s real. Those people are struggling in a way that they wouldn’t” because of climbing temperatures, he said. “Climate change right now is a threat multiplier — it makes bad things worse.”
Lemery and Prunicki are among the doctors planning to organize events in their respective regions to educate peers about climate-related threats to patients’ health, through the Climate Crisis and Clinical Practice Initiative, the effort launched in Boston in February.
“There are so many really brilliant, smart clinicians who have no clue” about the link between climate change and human health, said Lemery, who has also written a textbook and started a fellowship on the topic.
Salas said she sometimes hears pushback that climate change is too political for the exam room. But despite misleading information from the fossil fuel industry, she said, the science is clear. Based on the evidence, 97 percent of climate scientists agree that humans are causing global warming.
Salas said that, as she sat with the distraught mother of the 4-year-old girl with asthma in Boston, her decision to broach the topic was easy.
“Of course I have to talk to her about climate change,” Salas said, “because it’s impairing her ability to care for her daughter.”
Melissa Bailey is a reporter for Kaiser Health News.
Melissa Bailey: @mmbaily
Latest wrap-up of region's COVID-19 response
The front entrance of MGH, in Boston
Here is the most recent wrap-up the region’s COVID-19 developments from The New England Council (newenglandcouncil.com):
“Harvard Medical School Researchers Publish COVID-19 Rehabilitation Study – Researchers at Harvard Medical School have published a study detailing rehabilitation plans crafted for patients in Boston and New York-based hospitals. The team has treated over 100 patients and points to continued studies to address persistent COVID-19 symptoms. Read more here.
“Mass General Releases Guidance on Weaning Patients Off Ventilators – Clinicians at Massachusetts General Hospital have released an article with an accompanying video to demonstrate effective ways to wean patients with serious COVID-19 infections off of ventilators. The materials offer step-by-step instructions and were published in The New England Journal of Medicine. Read more here.
“Health Leads Releases Joint Statement on Ensuring Racial Equity in the Creation and Distribution of a COVID-19 Vaccine – Health Leads has released a statement, in conjunction with a number of other organizations and individuals, emphasizing the importance of supporting underserved communities in recovering from COVID-19. The statement includes strategies for ensuring equity in vaccine distribution. Read more here.’’
Study: Most Boston area COVID-19 infections came from Europe
The Marriott Long Wharf Hotel in Boston, the site of a Biogen international meeting on Feb. 26-28 to which most early COVID-19 cases in Massachusetts have been traced.
From The New England Council (newenglandcouncil.com)
“Researchers at Massachusetts General Hospital (MGH) have published a draft of a new report tracing the beginnings of the outbreak of COVID-19 in the United States, especially in the Boston area. The report concludes that, in Greater Boston, most infections came from Western Europe. Read more from WBUR.’’
Map of the outbreak in Massachusetts by confirmed infections per 100,000 people (as of June 10). The darker the color, the more intense the case load.
N.E. responds to COVID-19: A testing site for uninsured; policy-change simulator; in-state tuition for out-of staters
The First Congregation Church in Boston’s Hyde Park neighborhood, whose unofficial motto is “A Small Town in the City.’’ A mobile COVID-19 testing site has been opened there for the uninsured.
From The New England Council (newenglandcouncil.com)
BOSTON
As our region and our nation continue to grapple with the Coronavirus Disease (COVID-19) pandemic, The New England Council is using our blog as a platform to highlight some of the incredible work our members have undertaken to respond to the outbreak. Each day, we’ll post a round-up of updates on some of the initiatives underway among Council members throughout the region. We are also sharing these updates via our social media, and encourage our members to share with us any information on their efforts so that we can be sure to include them in these daily roundups.
You can find all the Council’s information and resources related to the crisis in the special COVID-19 section of our Web site. This includes our COVID-19 Virtual Events Calendar, which provides information on upcoming COVID-19 Congressional town halls and webinars presented by NEC members, as well as our newly-released Federal Agency COVID-19 Guidance for Businesses page.
Here is the April 27 roundup
Medical Response
Brigham and Women’s Hospital Opens Mobile Testing Site for Uninsured – In Hyde Park—one of Boston’s emerging virus hotspots—Brigham and Women’s Hospital has opened a mobile testing site to serve those with coronavirus symptoms but without health insurance. Testing at the site will be free of charge, and providers will not ask patients about immigration status. The testing site will also provide masks, boxes of food, and educational materials for those who qualify. Read more from CBS Boston.
Massachusetts General Hospital Researchers Develop Simulator to Predict Policy Change Effects – As states weigh when and how to begin re-opening nonessential businesses, Massachusetts General Hospital (MGH) has built a COVID-19 simulator to predict infections, hospitalizations, and deaths from coronavirus in the state under different plans of action. The model uses virus data to create statistical predictions of the its spread to inform state and local leaders on when it will be safe to ease physical distancing regulations. WBUR has more.
Economic/Business Continuity Response
The University of Maine Offers Tuition Break for Students Affected by Coronavirus – To support students across the country facing educational uncertainty, the University of Maine (UMaine) has launched a new initiative, The Maine Welcome, to allow all students—regardless of state origin—to pay in-state tuition to continue their studies. The program aims to help students as they navigate potential school closures and revenue losses. More from Mainebiz
PwC Makes Digital Fitness App Free Worldwide – To allow workers across sectors and around the world to develop digital skills, PricewaterhouseCoopers (PwC) has made its technological training app free globally. The app offers courses and learning assessments to instruct workers to learn important skills in a workforce increasingly dependent on technology. Cyprus Mail has more.
Community Response
AAA Northeast Uses Service Fleet to Deliver Protective Gear – In partnership with a West Haven, Conn., manufacturer, AAA Northeast is utilizing its fleet of service vehicles, deemed essential, to deliver gowns and other protective equipment made by Thermaxx to first responders and Connecticut state agencies. Read more in WTNH.
Harvard Pilgrim Health Care Enters Partnership to Provide Meals to Families – Harvard Pilgrim Health Care has donated $52,000 to sponsor a month of free meals for families through the Dimock Center. The Dimock Center will provide meals twice a week for families for one month using the donation, but Harvard Pilgrim has committed to additional funding as needed. The Jamaica Plain Gazette has more.
Boeing Transports 1.5 Million Masks to Aid Response – Continuing its relief missions around the world, Boeing delivered 1.5 million face masks from Hong Kong to the United States. The protective equipment will be used by healthcare providers across the country to combat shortages of the equipment necessary to keep healthcare workers safe. Read the release here.
Stay tuned for more updates each day, and follow us on Twitter for more frequent updates on how Council members are contributing to the response to this global health crisis.
Melissa Bailey: Even in New England, global warming putting physicians in hot seat
Person being cooled with water spray, one of the treatments of heat stroke in Iraq in 1943
BOSTON
A 4-year-old girl was rushed to the emergency room three times in one week for asthma attacks.
An elderly man, who’d been holed up in a top-floor apartment with no air conditioning during a heat wave, showed up at a hospital with a temperature of 106 degrees.
A 27-year-old man arrived in the ER with trouble breathing ― and learned he had end-stage kidney disease, linked to his time as a sugar cane farmer in the sweltering fields of El Salvador.
These patients, whose cases were recounted by doctors, all arrived at Boston-area hospitals in recent years. While the coronavirus pandemic is at the forefront of doctor-patient conversations these days, there’s another factor continuing to shape patients’ health: climate change.
Global warming is often associated with dramatic effects such as hurricanes, fires and floods, but patients’ health issues represent the subtler ways that climate change is showing up in the exam room, according to the physicians who treated them.
Dr. Renee Salas, an emergency physician at Massachusetts General Hospital, said she was working a night shift when the 4-year-old arrived the third time, struggling to breathe. The girl’s mother felt helpless that she couldn’t protect her daughter, whose condition was so severe that she had to be admitted to the hospital, Salas recalled.
She found time to talk with the patient’s mother about the larger factors at play: The girl’s asthma appeared to be triggered by a high pollen count that week. And pollen levels are rising in general because of higher levels of carbon dioxide, which she explained is linked to human-caused climate change.
Salas, a national expert on climate change and health, is a driving force behind an initiative to spur clinicians and hospitals to take a more active role in responding to climate change. The effort launched in Boston in February, and organizers aim to spread it to seven U.S. cities and Australia over the next year and a half.
Although there is scientific consensus on a mounting climate crisis, some people reject the idea that rising temperatures are linked to human activity. The controversy can make doctors hesitant to bring it up.
Even at the climate change discussion in Boston, one panelist suggested the topic may be too political for the exam room. Dr. Nicholas Hill, head of the Pulmonary, Critical Care and Sleep Division at Tufts Medical Center of Medicine, recalled treating a “cute little old lady” in her 80s who likes Fox News, a favorite of climate change doubters. With someone like her, talking about climate change may hurt the doctor-patient relationship, he suggested. “How far do you go in advocating with patients?”
Doctors and nurses are well suited to influence public opinion because the public considers them “trusted messengers,” said Dr. Aaron Bernstein, who co-organized the Boston event and co-directs the Center for Climate, Health, and the Global Environment at Harvard’s school of public health. People have confidence they will provide reliable information when they make highly personal and even life-or-death decisions.
Bernstein and others are urging clinicians to exert their influence by contacting elected officials, serving as expert witnesses, attending public protests and reducing their hospital’s carbon emissions. They’re also encouraging them to raise the topic with patients.
Dr. Mary Rice, a pulmonologist who researches air quality at Beth-Israel Deaconess Medical Center here, recognized that in a 20-minute clinic visit, doctors don’t have much time to spare.
But “I think we should be talking to our patients about this,” she said. “Just inserting that sentence, that one of the reasons your allergies are getting worse is that the allergy season is worse than it used to be, and that’s because of climate change.”
Salas, who has been a doctor for seven years, said she had little awareness of the topic until she heard climate change described as the “greatest public health emergency of our time” during a 2013 conference.
“I was dumbfounded about why I hadn’t heard of this, climate change harming health,” she said. “I clearly saw this is going to make my job harder” in emergency medicine.
Now, Salas said, she sees ample evidence of climate change in the exam room. After Hurricane Maria devastated Puerto Rico, for instance, a woman seeking refuge in Boston showed up with a bag of empty pill bottles and thrust it at Salas, asking for refills, she recalled. The patient hadn’t had her medications replenished for weeks because of the storm, whose destructive power was likely intensified by climate change, according to scientists.
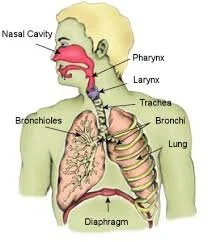
Climate change presents many threats across the country, Salas noted: Heat stress can exacerbate mental illness, prompt more aggression and violence, and hurt pregnancy outcomes. Air pollution worsens respiratory problems. High temperatures can weaken the effectiveness of medications such as albuterol inhalers and EpiPens.
The delivery of health care is also being disrupted. Disasters like Hurricane Maria have caused shortages in basic medical supplies. Last November, nearly 250 California hospitals lost power in planned outages to prevent wildfires. Natural disasters can interrupt the treatment of cancer, leading to earlier death.
Even a short heat wave can upend routine care: On a hot day last summer, for instance, power failed at Mount Auburn Hospital in Cambridge, Massachusetts, and firefighters had to move patients down from the top floor because it was too hot, Salas said.
Other effects of climate change vary by region. Salas and others urged clinicians to look out for unexpected conditions, such as Lyme disease and West Nile virus, that are spreading to new territory as temperatures rise.
In California, where wildfires have become a fact of life, researchers are scrambling to document the ways smoke inhalation is affecting patients’ health, including higher rates of acute bronchitis, pneumonia, heart attacks, strokes, irregular heartbeats and premature births.
Researchers have shown that heavy exposure to wildfire smoke can change the DNA of immune cells, but they’re uncertain whether that will have a long-term impact, said Dr. Mary Prunicki, director of air pollution and health research at Stanford University’s center for allergy and asthma research.
“It causes a lot of anxiety,” Prunicki said. “Everyone feels helpless because we simply don’t know — we’re not able to give concrete facts back to the patient.”
In Denver, Dr. Jay Lemery, a professor of emergency medicine at the University of Colorado School of Medicine, said he’s seeing how people with chronic illnesses like diabetes and chronic obstructive pulmonary disease suffer more with extreme heat.
There’s no medical code for “hottest day of the year,” Lemery said, “but we see it; it’s real. Those people are struggling in a way that they wouldn’t” because of climbing temperatures, he said. “Climate change right now is a threat multiplier — it makes bad things worse.”
Lemery and Prunicki are among the doctors planning to organize events in their respective regions to educate peers about climate-related threats to patients’ health, through the Climate Crisis and Clinical Practice Initiative, the effort launched in Boston in February.
“There are so many really brilliant, smart clinicians who have no clue” about the link between climate change and human health, said Lemery, who has also written a textbook and started a fellowship on the topic.
Salas said she sometimes hears pushback that climate change is too political for the exam room. But despite misleading information from the fossil fuel industry, she said, the science is clear. Based on the evidence, 97% of climate scientists agree that humans are causing global warming.
Salas said that, as she sat with the distraught mother of the 4-year-old girl with asthma in Boston, her decision to broach the topic was easy.
“Of course I have to talk to her about climate change,” Salas said, “because it’s impairing her ability to care for her daughter.”
Melissa Bailey is a Kaiser Health News journalist.
Melissa Bailey: @mmbaily
Nitric oxide to treat COVID-19? Google-Apple project; convention center as hospital
Boston Convention and Exhibition Center has been transformed (temporarily!) into a medical center for COVID-19 patients.
From The New England Council (newenglandcouncil.com)
As our region and our nation continue to grapple with the Coronavirus Disease (COVID-19) pandemic, The New England Council is using our blog as a platform to highlight some of the incredible work our members have undertaken to respond to the outbreak. Each day, we’ll post a round-up of updates on some of the initiatives underway among Council members throughout the region. We are also sharing these updates via our social media, and encourage our members to share with us any information on their efforts so that we can be sure to include them in these daily round-ups.
You can find all the Council’s information and resources related to the crisis in the special COVID-19 section of our website. This includes our COVID-19 Virtual Events Calendar, which provides information on upcoming COVID-19 Congressional town meetings.
Here is the Aug. 13 roundup:
Medical Response
Massachusetts General Hospital Studying Possible Treatment – Researchers at Massachusetts General Hospital (MGH) are investigating whether the gas nitric oxide can help treat—or even prevent—COVID-19 infections. The gas, widely used for patients in respiratory failure, has been known to provide additional antiviral effects. The trial at MGH is the only in the country and one of few worldwide. Read more from WBUR.
Google Developing Contact-Tracing Technology – Google, in partnership with Apple, is working to develop technology to alert individuals if they have come into contact with someone infected with COVID-19. The technology will use contact tracing via Bluetooth signals to determine users that may have been in contact with infected individuals. To maintain privacy, the app would not record GPS location data or personal information. BBC News has more.
Sanofi Donates 100 Million Doses of Potential Treatment to 50 Countries – After its drug hydroxychloroquine emerged as a potential treatment for COVID-19, drugmaker Sanofi has pledged 100 million doses of the antimalarial drug across 50 countries. In addition to increasing production capacity of the drug, Sanofi has called for coordination and stabilization along the supply chain of the drug to quadruple production should hydroxychloroquine emerge as an effective treatment. More from Reuters.
Boston Convention and Exhibition Center Transformed into Medical Center – The Boston Convention and Exhibition Center—owned by the Massachusetts Convention Center Authority (MCCA)—has been transformed into a new medical center for COVID-19 patients. The facility, renamed Boston Hope Medical Center, will provide 1,000 beds and other resources for the city’s infected, and will be managed by Partners HealthCare and Boston Health Care for the Homeless. Read more in The Boston Globe.
Economic/Business Continuity Response
Dell Provides Early Payouts for Development Projects – To assist its research and development partners, Dell Technologies is offering cash payouts for development projects, as well as free training for services necessary to maintain operations. In addition, the tech company is providing no-interest loans and up to nine months of payment deferrals for its customers. CRN has more.
AT&T Technology Used to Help Disinfect Hospitals – AT&T, using its Internet of Things (IoT) technology, is partnering with technology companies to destroy viruses, bacteria, and spores on surfaces in hospitals. The connectivity from AT&T allows the technology to use ultraviolet (UV) rays to disinfect surfaces and helps the technology optimize performance, lower healthcare costs, and maximize patient and worker safety in hospitals. Read more.
Community Response
Boston Colleges Offer Residence Halls to Exposed Workers – Supporting a wide variety of employees from facilities ranging from the Pine Street Inn and Brigham and Women’s Hospital, Boston-area colleges are offering their residence halls and campus facilities to workers who might have been exposed to the novel coronavirus. Northeastern University, Emmanuel College, Boston University, Simmons University, and Massachusetts College of Art and Design are some of the schools offering support to workers across multiple industries to protect them. Read more from WBUR.
Veolia Donates 40,000 Masks to Hospitals –Environmental services company Veolia has donated 40,000 masks to hospitals across the United States and Canada, drawing from its existing stockpile. The masks will provide exposed workers with the protective equipment they need to remain safe while working. The Post Star has more.
Stay tuned for more updates each day, and follow us on Twitter for more frequent updates on how Council members are contributing to the response to this global health crisis.
Boston hospitals unite to handle influx; UMaine offering online campus tours for prospective students; race track speeds PPE’s
This is from our friends at The New England Council (newenglandcouncil.com):
As our region and our nation continue to grapple with the Coronavirus Disease (COVID-19) pandemic, The New England Council is using our blog as a platform to highlight some of the work our members have undertaken to respond to the outbreak. Each day, we’ll post a round-up of updates on some of the initiatives underway among Council members throughout the region. We are also sharing these updates via our social media, and encourage our members to share with us any information on their efforts so that we can be sure to include them in these daily round-ups.
You can find all the Council’s information and resources related to the crisis in the special COVID-19 section of our Web site. This includes our COVID-19 Virtual Events Calendar, which provides information on upcoming COVID-19 Congressional town halls and webinars presented by NEC members, as well as our newly-released Federal Agency COVID-19 Guidance for Businesses page.
Here is today’s (April 10, 2020) roundup:
Medical Response
Boston Hospitals Launch Citywide Group to Manage Influx – To better coordinate the handling of incoming patients, Massachusetts General Hospital (MGH) and Beth Israel Deaconess Medical Center (BIDMC) are jointly leading a response group across Boston. The group streamlines the flow of patients to hospitals in the group to avoid moving staff and resources, with support from The Massachusetts Health & Hospital Association as well as a growing network of the city’s hospitals. WBUR has more.
MIT Contact Tracing App Adopted by Local Governments – Three local government entities plan to introduce Private Kit, an app developed by Massachusetts Institute of Technology (MIT) researchers. The app allows for extensive – yet still private– “contact tracing” using users’ Bluetooth signals. Other counties and municipalities around the country are considering introducing the app in their communities in the coming weeks. Read more in Reuters.
Beth Israel Doctors Begin Testing Drug to Reduce Need for Ventilators – Doctors at Beth Israel Deaconess Medical Center have launched clinical trials to test tPA to treat COVID-19 related respiratory failure, thereby reducing the demand for ventilators. The anti-clotting drug is usually reserved for heart attack and stroke patients, but after some initial success in treating coronavirus patients, will now enter a two-phase clinical trial. Read the press release here.
A tree-lined path through the Lyle E. Littlefield Ornamental Gardens, at the University of Maine’s flagship campus, in Orono. The university provides online tours to prospective students.
The New Hampshire Motor Speedway, in Loudon, the biggest such operation in New England by far. It’s donating PPE’s.
Economic/Business Continuity Response
UMaine Utilizing Virtual Programming for Prospective Students – While high school seniors are unable to visit campuses as they choose where to attend college, the University of Maine (UMaine) is offering virtual programs, such as campus tours and videoconferencing options with professors, to highlight the resources of the university. Read more in the Bangor Daily News.
New England Center for Children Maintains Residential Program – The New England Center for Children (NECC) in Framingham continues to operate its residential educational program for children with autism amid the pandemic. Many of the students who reside at the center cannot safely return to their homes To support these students and ensure they have adequate resources and assistance during the pandemic, NECC’s residential program—with the support of the state of Massachusetts—continues to keep their students safe while meeting their diverse needs. Read more from WBUR
Community Response
Massachusetts Hospitals Receive Part of $38 Million Relief Donation – UMass Memorial Medical Center, in Worcester, and Massachusetts General Hospital in Boston are among the recipients of $2.3 in aid to Massachusetts relief efforts from insurance company MAPFRE. The funds are part of a $38 million aid package donated by the Spanish insurer to aid in COVID-19 relief efforts. Several other Massachusetts hospitals will also receive a share of the funds. Read more in The Worcester Business Journal.
New Hampshire Motor Speedway Donates Protective Equipment – The New Hampshire Motor Speedway has donated 800 units of personal protective equipment (PPE) for local health-care workers in the state. The NASCAR track donated the items directly to the city of Loudon, N.H., where the track is situated. Read more from NBC Sports.
UnitedHealth Group Pledges $50 Million for Relief Efforts – Supporting those most directly affected by the pandemic—ranging from hard-hit states to seniors and those experiencing food insecurity—UnitedHealth Group has committed $50 million toward relief efforts. Funds will be spread across the country to alleviate financial strain on these vulnerable populations. Read the release here.
Stay tuned for more updates each day, and follow us on Twitter for more frequent updates on how Council members are contributing to the response to this global health crisis.T
How microbiomes affect disease
Escherichia coli: a long-term resident in our gut
This is from the New England Council (newenglandcouncil.com):
"IBM and Massachusetts General Hospital (MGH) are joining forces to study how human microbiomes affect various diseases.
"In collaboration with the Broad Institute, the University of California {at} San Diego and the Simons Foundation’s Flatiron Institute, IBM and MGH will attempt to map the three million bacterial genes found in the human microbiome to further understand how to treat diseases such as Type 1 diabetes, Crohn’s disease, and ulcerative colitis. Research at this level is unprecedented and a massive amount of computing power is required for analysis which is where IBM’s 'citizen science' World Community Grid enters the picture. The World Community Grid is a hyper-secure software that can gauge when a personal computer has processing power to spare and then remotely run experiments for the project. Anyone with Internet can chose to contribute to the study by joining the Microbiome Immunity Project through IBM’s World Community Grid.
“'This type of research on the human microbiome, on this scale, has not been done before,' said Ramnik Xavier, co-director of the Infectious Disease and Microbiome Program at the Broad Institute of MIT and Harvard and chief of the gastrointestinal unit at MGH. 'It’s only possible with massive computational power.'''
Will hospital merger mania continue?
Excerpted from Robert Whitcomb's "Digital Diary,'' in GoLocal24.
The collapse of affiliation talks between Care New England, the Rhode Island hospital chain, and Southcoast Health, in southeastern Massachusetts, as did the collapse of Lifespan and Care New England talks a few years back, raises the question of when we’ll see another hospital chain merger around here, given the inevitable turf battles.
With the drive for economies of scale and for sharing access to the best care and research, will the latest collapse lead to a big Boston-based chain coming in and taking over? Partners HealthCare, whose hospitals include Massachusetts General Hospital and Brigham & Women’s, might eye expansion in these parts because Massachusetts regulators think that it has gotten too big and powerful in Greater Boston. The Brown Medical School would presumably not like a Partners invasion because Partners is joined at the hip with the Harvard Medical School behemoth. Maybe given the size and executive salaries of hospitals these days, affiliating with the Harvard Business School would be appropriate.
Many hospital chains want to merge to strengthen their bargaining power with huge insurance companies. Maybe in 10 years, we’ll have “Medicare for all,’’ which will make much of this moot.
In the meantime, we have something to learn from those independent hospitals, such as South County Hospital, in southern Rhode Island, that have maintained their independence and high-quality care in the face of the massive disruption that that healthcare sector is now undergoing.