Judith Graham: Patients sharply divided over Alzheimer’s drug
Self-portrait of American figurative artist William Utermohlen, created after he was diagnosed with Alzheimer's disease, in 1995. He experienced memory loss beginning in 1991. After his diagnosis he began creating self-portraits and continued it for another six years, until he made the final self-portraits in 2001. He died in 2007. In the years after the publication of his works in The Lancet in 2001, Utermohlen's self-portraits have been displayed in several exhibitions. His self-portraits inspired the 2019 short film Mémorable.
If you listen to the nation’s largest Alzheimer’s disease advocacy organizations, you might think everyone living with Alzheimer’s wants unfettered access to Aduhelm, a controversial new treatment produced by the Cambridge, Mass., biotech company Biogen.
But you’d be wrong.
Opinions about Aduhelm (also known as aducanumab) in the dementia community are diverse, ranging from “we want the government to cover this drug” to “we’re concerned about this medication and think it should be studied further.”
The Alzheimer’s Association and UsAgainstAlzheimer’s, the most influential advocacy organizations in the field, are in the former camp.
Both are pushing for Medicare to cover Aduhelm’s $28,000 annual per-patient cost and fiercely oppose the Centers for Medicare & Medicaid Services’ January proposal to restrict coverage only to people enrolled in clinical trials. Nearly 10,000 comments were received on that proposal, and a final decision is expected in April.
“With respect, we have no more time for debate or delay,” the Alzheimer’s Association national Early-Stage Advisory Group wrote in a Feb. 10 comment. “Every passing day without access to potential treatments subjects us to a future of irreversible decline.” For its part, UsAgainstAlzheimer’s called CMS’ proposal “anti-patient.”
Yet the scientific evidence behind Aduhelm is inconclusive, its efficacy in preventing the progression of Alzheimer’s remains unproved, and there are concerns about its safety. The FDA granted accelerated approval to the medication last June but ordered the drugmaker, Biogen, to conduct a new clinical trial to verify its benefit. And the agency’s decision came despite a 10-0 recommendation against doing so from its scientific advisory committee. (One committee member abstained, citing uncertainty.)
Other organizations representing people living with dementia are more cautious, calling for more research about Aduhelm’s effectiveness and potential side effects. More than 40 percent of people who take the medication have swelling or bleeding in the brain — complications that need to be carefully monitored.
The Dementia Action Alliance, which supports people living with dementia, is among them. In a statement forwarded to me by CEO Karen Love, the organization said, “DAA strongly supports CMS’s decision to limit access to aducanumab to people enrolled in qualifying clinical trials in order to better study aducanumab’s efficacy and adverse effects.”
Meanwhile, Dementia Alliance International — the world’s largest organization run by and for people with dementia, with more than 5,000 members — has not taken a position on Aduhelm. “We felt that coming out with a statement on one side or another would split our organization,” said Diana Blackwelder, its treasurer, who lives in Washington, D.C.
Blackwelder, 60, who was diagnosed with early-onset Alzheimer’s in 2017, told me, “To say that millions of people afflicted with a disease are all up in arms against CMS’s proposal is just wrong. We’re all individuals, not a collective.”
“I understand the need for hope,” she said, expressing a personal opinion, “but people living with dementia need to be protected as well. This drug has very serious, frequent side effects. My concern is that whatever CMS decides, they at least put in some guardrails so that people taking this drug get proper workups and monitoring.”
The debate over Medicare’s decision on Aduhelm is crucial, since most people with Alzheimer’s are older or seriously disabled and covered by the government health program.
To learn more, I talked to several people living with dementia. Here’s some of what they told me:
Jay Reinstein, 60, is married and lives in Raleigh, N.C. He was diagnosed with early-onset Alzheimer’s disease three years ago and formerly served on the national board of directors of the Alzheimer’s Association.
“I understand [Aduhelm] is controversial, but to me it’s a risk I’m willing to take because there’s nothing else out there,” Reinstein said, noting that people he’s met through support groups have progressed in their disease very quickly. “Even if it’s a 10 percent chance of slowing [Alzheimer’s] down by six months, I am still willing to take it. While I am progressing slowly, I want more time.”
Laurie Scherrer of Albertville, Ala., was diagnosed with early-onset Alzheimer’s and frontotemporal dementia in 2013, at age 55.
Early on, she was prescribed Aricept (donepezil), one of a handful of medications that address Alzheimer’s symptoms. “I became totally confused and disoriented, I couldn’t think, I couldn’t concentrate,” she told me. After stopping the medication, those symptoms went away.
“I am not for CMS approving this drug, and I wouldn’t take it,” Scherrer said. At discussion groups on Aduhelm hosted by the Dementia Action Alliance (Scherrer is on the board), only two of 50 participants wanted the drug to be made widely available. The reason, she said: “They don’t think there are enough benefits to counteract the possible harms.”
Rebecca Chopp, 69, of Broomfield, Colo., was diagnosed with early-onset Alzheimer’s in March 2019. She’s a former chancellor of the University of Denver.
Chopp is a member of a newly formed group of five people with dementia who meet regularly, “support one another,” and want to “tell the story of Alzheimer’s from our perspective,” she said.
Two people in the group have taken Aduhelm, and both report that it has improved their well-being. “I believe in science, and I am very respectful of the large number of scientists who feel that [Aduhelm] should not have been approved,” she told me. “But I’m equally compassionate toward those who are desperate and who feel this [drug] might help them.”
Chopp opposes CMS’s decision because “Aduhelm has been FDA-approved and I think it should be funded for those who choose to take it.”
Joanna Fix, 53, of Colorado Springs was diagnosed with early-onset Alzheimer’s disease in October 2016. She, too, developed serious complications after taking Aricept and another dementia medication, Namenda (memantine).
“I would love it if tomorrow somebody said, ‘Here’s something that can cure you,’ but I don’t think we’re at that point with Aduhelm,” Fix told me. “We haven’t been looking at this [drug] long enough. It feels like this is just throwing something at the disease because there’s nothing else to do.”
“Please, please take it from someone living with this disease: There is more to life than taking a magic pill,” Fix continued. “All I care about is my quality of life. My marriage. Educating and helping other people living with dementia. And what I can still do day to day.”
Phil Gutis, 60, of Solebury, Penn., has participated in clinical trials and taken Aduhelm for 5½ years after being diagnosed with early-onset Alzheimer’s in 2016.
He’s convinced the medication has helped him. “I don’t know how to describe it other than to say my head feels so much clearer now,” he told me. “I feel much more capable of doing things now. It’s not like I’ve gained my memories back, but I certainly haven’t deteriorated.”
Gutis thinks CMS’s proposed restrictions on Aduhelm are misguided. “When the FDA approved it, there was this sense of excitement — oh, we’re getting somewhere. With the CMS decision, I feel we are setting the field back again. It’s this constant feeling that progress is being made and then — whack.”
Christine Thelker, 62, is a widow who lives alone in Vernon, British Columbia. She was diagnosed with vascular dementia seven years ago and is a board member for Dementia Advocacy Canada, which supports restrictions on Aduhelm’s availability.
“Most of us who live with dementia understand a cure is not likely: There are too many different types of dementia, and it’s just too complicated,” Thelker told me. “To think we’re just going to take a pill and be better is not realistic. Don’t give us false hope.”
What people with Alzheimer’s and other types of dementia need, instead, is “various types of rehabilitation and assistance that can improve our quality of life and help us maintain a sense of hope and purpose,” Thelker said.
Jim Taylor of New York City and Sherman, Conn., is a caregiver for his wife, Geri Taylor, 78, who has moderate Alzheimer’s. She joined a clinical trial for Aduhelm in 2015 and has been on the drug since, with the exception of about 12 months when Biogen temporarily stopped the clinical trial. “In that period, her short-term memory and communications skills noticeably declined,” Jim Taylor said.
“We’re convinced the medication is a good thing, though we know it’s not helpful for everybody,” Taylor continued. “It really boosts [Geri’s] spirits to think she’s part of research and doing everything she can.
“If it’s helpful for some and it can be monitored so that any side effects are caught in a timely way, then I think [Aduhelm] should be available. That decision should be left up to the person with the disease and their care partner.”
Judith Graham is a Kaiser Health News reporter.
Biogen headquarters in Cambridge, one of the world’s biotech centers.
Judith Graham: With the arrival of Aduhelm, what is 'mild cognitive impairment'?
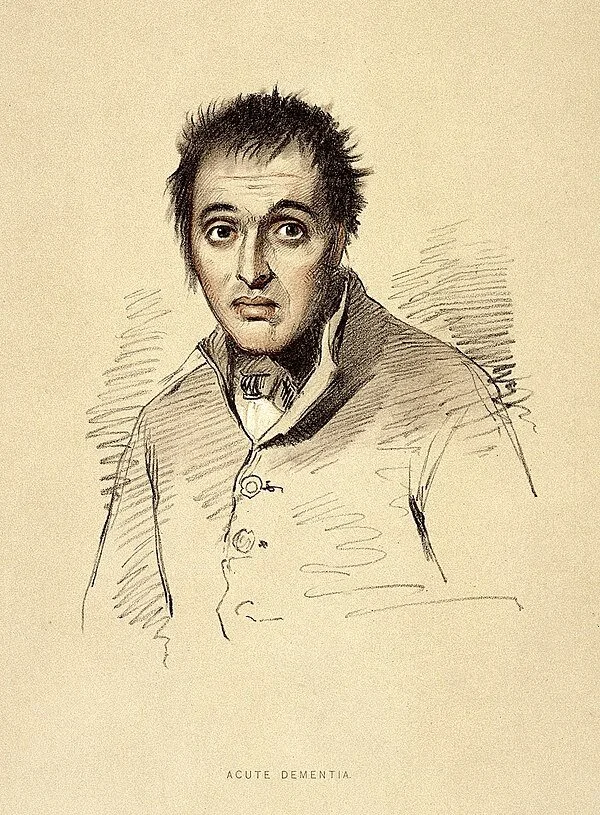
19th Century drawing of man with dementia
The approval of a controversial new drug for Alzheimer’s disease, Aduhelm, made by Cambridge, Mass.-based Biogen, is shining a spotlight on mild cognitive impairment — problems with memory, attention, language or other cognitive tasks that exceed changes expected with normal aging.
(Kendall Square in Cambridge, Biogen’s neighborhood, has become arguably the bio-tech center of the world.)
After initially indicating that it could be prescribed to anyone with dementia, the Food and Drug Administration now specifies that the prescription drug be given only to individuals with mild cognitive impairment or early-stage Alzheimer’s, the groups in which the medication was studied.
Yet this narrower recommendation raises questions. What does a diagnosis of mild cognitive impairment mean? Is Aduhelm appropriate for all people with mild cognitive impairment, or only some? And who should decide which patients qualify for treatment: dementia specialists or primary-care physicians?
Controversy surrounds Aduhelm because its effectiveness hasn’t been proved, its cost is high (an estimated $56,000 a year, not including expenses for imaging and monthly infusions), and its potential side-effects are significant (41 percent of patients in the drug’s clinical trials experienced brain swelling and bleeding).
Furthermore, an FDA advisory committee strongly recommended against Aduhelm’s approval, and Congress is investigating the process leading to the FDA’s decision. Medicare is studying whether it should cover the medication, and the Department of Veterans Affairs has declined to do so under most circumstances.
Clinical trials for Aduhelm excluded people over age 85; those taking blood thinners; those who had experienced a stroke; and those with cardiovascular disease or impaired kidney or liver function, among other conditions. If those criteria were broadly applied, 85 percent of people with mild cognitive impairment would not qualify to take the medication, according to a new research letter in the Journal of the American Medical Association.
Given these considerations, carefully selecting patients with mild cognitive impairment who might respond to Aduhelm is “becoming a priority,” said Dr. Kenneth Langa, a professor of medicine, health management and policy at the University of Michigan.
Dr. Ronald Petersen, who directs the Mayo Clinic’s Alzheimer’s Disease Research Center, said, “One of the biggest issues we’re dealing with since Aduhelm’s approval is, ‘Are appropriate patients going to be given this drug?’”
Here’s what people should know about mild cognitive impairment based on a review of research studies and conversations with leading experts:
Basics. Mild cognitive impairment is often referred to as a borderline state between normal cognition and dementia. But this can be misleading. Although a significant number of people with mild cognitive impairment eventually develop dementia — usually Alzheimer’s disease — many do not.
Cognitive symptoms — for instance, difficulties with short-term memory or planning — are often subtle but they persist and represent a decline from previous functioning. Yet a person with the condition may still be working or driving and appear entirely normal. By definition, mild cognitive impairment leaves intact a person’s ability to perform daily activities independently.
According to an American Academy of Neurology review of dozens of stuies, published in 2018, mild cognitive impairment affects nearly 7 percent of people ages 60 to 64, 10 percent of those 70 to 74 and 25 percent of 80-to-84-year-olds.
Causes. Mild cognitive impairment can be caused by biological processes (the accumulation of amyloid beta and tau proteins and changes in the brain’s structure) linked to Alzheimer’s disease. Between 40 percent and 60 percent of people with mild cognitive impairment have evidence of Alzheimer’s-related brain pathology, according to a 2019 review.
But cognitive symptoms can also be caused by other factors, including small strokes; poorly managed conditions, such as diabetes, depression and sleep apnea; responses to medications; thyroid disease; and unrecognized hearing loss. When these issues are treated, normal cognition may be restored or further decline forestalled.
Subtypes. During the past decade, experts have identified four subtypes of mild cognitive impairment. Each subtype appears to carry a different risk of progressing to Alzheimer’s disease, but precise estimates haven’t been established.
People with memory problems and multiple medical issues who are found to have changes in their brain through imaging tests are thought to be at greatest risk. “If biomarker tests converge and show abnormalities in amyloid, tau and neuro-degeneration, you can be pretty certain a person with MCI has the beginnings of Alzheimer’s in their brain and that disease will continue to evolve,” said Dr. Howard Chertkow, chairperson for cognitive neurology and innovation at Baycrest, an academic health-sciences center in Toronto that specializes in care for older adults.
Diagnosis. Usually, this process begins when older adults tell their doctors that “something isn’t right with my memory or my thinking” — a so-called subjective cognitive complaint. Short cognitive tests can confirm whether objective evidence of impairment exists. Other tests can determine whether a person is still able to perform daily activities successfully.
More sophisticated neuropsychological tests can be helpful if there is uncertainty about findings or a need to better assess the extent of impairment. But “there is a shortage of physicians with expertise in dementia — neurologists, geriatricians, geriatric psychiatrists” — who can undertake comprehensive evaluations, said Kathryn Phillips, director of health services research and health economics at the University of California-San Francisco School of Pharmacy.
The most important step is taking a careful medical history that documents whether a decline in functioning from an individual’s baseline has occurred and investigating possible causes such as sleep patterns, mental health concerns and inadequate management of chronic conditions that need attention.
Mild cognitive impairment “isn’t necessarily straightforward to recognize, because people’s thinking and memory changes over time [with advancing age] and the question becomes ‘Is this something more than that?’” said Dr. Zoe Arvanitakis, a neurologist and director of Rush University’s Rush Memory Clinic, in Chicago.
More than one set of tests is needed to rule out the possibility that someone performed poorly because they were nervous or sleep-deprived or had a bad day. “Administering tests to people over time can do a pretty good job of identifying who’s actually declining and who’s not,” Langa said.
Progression. Mild cognitive impairment doesn’t always progress to dementia, nor does it usually do so quickly. But this isn’t well understood. And estimates of progression vary, based on whether patients are seen in specialty dementia clinics or in community medical clinics and how long patients are followed.
A review of 41 studies found that 5 percent of patients treated in community settings each year went on to develop dementia. For those seen in dementia clinics — typically, patients with more serious symptoms — the rate was 10 percent. The American Academy of Neurology’s review found that after two years 15 percent of patients were observed to have dementia.
Progression to dementia isn’t the only path that people follow. A sizable portion of patients with mild cognitive impairment — from 14 percent to 38 percent — are discovered to have normal cognition upon further testing. Another portion remains stable over time. (In both cases, this may be because underlying risk factors — poor sleep, for instance, or poorly controlled diabetes or thyroid disease — have been addressed.) Still another group of patients fluctuate, sometimes improving and sometimes declining, with periods of stability in between.
“You really need to follow people over time — for up to 10 years — to have an idea of what is going on with them,” said Dr. Oscar Lopez, director of the Alzheimer’s Disease Research Center at the University of Pittsburgh.
Specialists versus generalists. Only people with mild cognitive impairment associated with Alzheimer’s should be considered for treatment with Aduhelm, experts agreed. “The question you want to ask your doctor is, ‘Do I have MCI [mild cognitive impairment] due to Alzheimer’s disease?’” Chertkow said.
Because this medication targets amyloid, a sticky protein that is a hallmark of Alzheimer’s, confirmation of amyloid accumulation through a PET scan or spinal tap should be a prerequisite. But the presence of amyloid isn’t determinative: One-third of older adults with normal cognition have been found to have amyloid deposits in their brains.
Because of these complexities, “I think, for the early rollout of a complex drug like this, treatment should be overseen by specialists, at least initially,” said Petersen of the Mayo Clinic. Arvanitakis of Rush University agreed. “If someone is really and truly interested in trying this medication, at this point I would recommend it be done under the care of a psychiatrist or neurologist or someone who really specializes in cognition,” she said.
Judith Graham is a Kaiser Health News reporter.
Judith Graham: khn.navigatingaging@gmail.com, @judith_graham